The scientific community faces unique complexities in the quest for an HIV vaccine. José Alcamí Pertejo, coordinator of the Spanish Network on AIDS Research, and Josep Mallolas, head of the HIV-AIDS Unit at the Hospital Clínic de Barcelona, explain in this article what makes the virus so resilient and why we were able to achieve immunization against COVID-19 but not for HIV?
A vaccine against HIV, a challenging journey
When we give a talk about the HIV vaccine, the most common question is: How was it possible to develop a vaccine against COVID-19 in less than a year, and after four decades, we still don’t have one for HIV? Besides feeling somewhat awkward, we try to explain that these two viruses cannot be compared. HIV represents a completely new challenge in the field of vaccines.
First and foremost, let’s clarify what a vaccine is: we’re talking about a biological simulation where we expose our immune system to the simulated attack of a microbe. Thanks to this simulation, our system activates and stores the germ we vaccinated against in its memory. When we later face a real infection, the trained system remembers, recognizes, and eliminates the microbe.
A series of failures
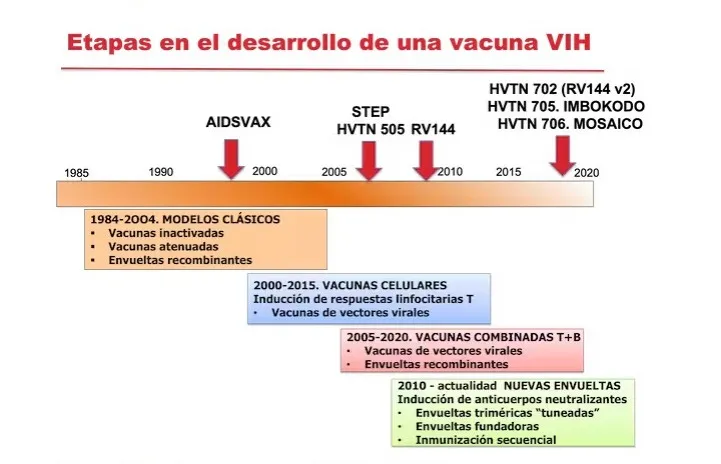
In the case of vaccines developed against HIV, we can distinguish three stages.
Initially, prototypes similar to classic vaccines for other viruses like polio and hepatitis B were used. These immunizations induce antibodies, biological missiles that block viruses before they enter our cells.
Faced with their failure, in a second stage, attempts were made to induce so-called cellular responses, the infantry that destroys infected cells. These prototypes also failed.
In the third stage, both strategies were combined: vaccines inducing antibodies and cellular responses. A positive result was achieved in one of these trials, RV144 (conducted in Thailand). But it was insufficient: only 30% of vaccinated subjects achieved protection when the minimum required is 50%. Moreover, it was not replicated in a similar trial in South Africa.
We can say that HIV has left the vaccine history strewn with the corpses of clinical trial names. Recently suspended for its lack of efficacy, Janssen’s Mosaico study has been the latest. No more Phase III trials are planned.
Why have we failed?
The biggest limitation in obtaining the vaccine is that our immune system is not prepared to face HIV. It’s easy to understand with an example. What happens when we get infected with COVID? If we’re not among the 1% of fatalities, we’ll recover in 99% of cases because our immune system eliminates the virus in a few days. In contrast, of 100 people infected with HIV, none can eliminate the virus. In the absence of treatment, 99 out of those 100 will die of AIDS.
We face a new challenge: teaching the immune system to do something it doesn’t naturally know how to do. Waking up the response, as traditional vaccines do, is insufficient because that reaction doesn’t work. We have to instruct the immune system to do something new that is effective.
What makes HIV so resistant to the immune response?
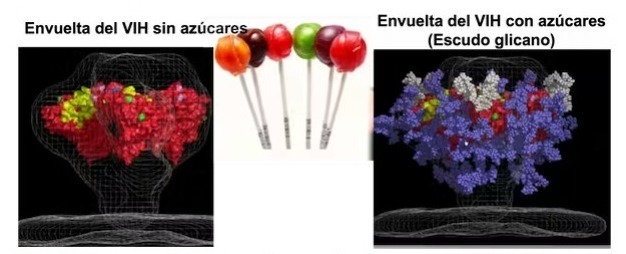
Evolution has provided HIV with a diabolical envelope or wrapper. The proteins of this covering are on the virus’s surface and allow it to infect cells by binding to cellular receptors. A vaccine is effective only if it induces antibodies that block these proteins, preventing the virus’s entry. These are called neutralizing antibodies. The envelope of HIV escapes these antibodies through four mechanisms.
- Differences between the envelopes of HIV and SARS-CoV-2 viruses. It forms a closed, inaccessible structure. Imagine antibodies aimed at the fingers of a hand. The envelope of SARS-CoV-2 is an open hand with easily reachable fingers, while that of HIV is a closed fist that only opens when it touches the cell membrane. It is too late for antibodies to reach their target.
- Like the shields of the spaceships in Star Wars, HIV covers its envelope with sugars that block the arrival of antibodies to its surface. It’s like a lollipop protecting its chocolate core inside.
- In the outer regions, accessible to antibodies, the envelope protein is highly variable, mutates, and escapes their attack.
- To these limitations is added that our immune system is slow against HIV. It needs two years to generate potent antibodies, and the virus produces resistant variants. In the race between antibodies and the envelope, HIV runs much faster.
Real-life difficulties in testing vaccines
In addition to the technical difficulty of obtaining a prototype vaccine with a chance of success, the difficulty of investigating the effectiveness of these prototypes in clinical practice is added. This is basically due to three reasons:
- The attack rate (new infections) is low, so cohorts of thousands of patients need to be followed for years to find significant differences between the vaccinated and placebo groups.
- Vaccines must be evaluated in populations with a higher likelihood of infection, such as those in sub-Saharan Africa, places with fragile health structures.
- From an ethical standpoint, participants must be offered and reminded to use protective measures, condoms…This reduces the number of infections and makes it more difficult to obtain differences between groups.
Is there any good news, or should we give up?
Although it may be hard to believe, there is good news.
Firstly, despite its hermeticism, we’ve found small cracks in the envelope of HIV. Some very special antibodies, which we call ‘broadly neutralizing,’ can reach these Achilles’ heels of the virus and block it.
Although very rare, these antibodies exist and are produced by some patients. Since we know which region of the HIV envelope they target, we can modify and fine-tune it to generate vaccines that induce these antibodies.
The final challenge is to produce these antibodies quickly. It’s possible to do so by immunizing sequentially with different envelope protein variants. This strategy accelerates the maturation of antibodies produced by the immune system.
Mission impossible?
We need vaccines capable of activating the scarce cells that produce these exceptional antibodies, capable of crossing the virus’s barriers and reaching its Achilles’ heels. Powerful antibodies that can neutralize hundreds of variants must be produced in weeks instead of taking years to generate. These are entirely new vaccines for a new problem, with a highly technological design. The vaccine against SARS-CoV-2 is a walk in the park compared to HIV, a summit of enormous difficulty.
In 2020, 1.5 million people were infected with HIV, and 680,000 died of AIDS. The virus is there, and it continues to kill. Developing a vaccine is the only way to end it. As difficult as it may be, we must keep trying. In his book The Art of War Sun Tzu says: ‘If you know your enemy and know yourself, you need not fear the result of a hundred battles. If you know neither the enemy nor yourself, you will succumb in every battle.’
Thanks to our failures, we know our weaknesses and the enemy’s strengths. Perhaps for the first time, we have a chance to win with the new generations of design vaccines we’re working on. (The Conversation)