“This has been the most horrendous experience of my life. There’s no other way of explaining it.” These were Alicia’s first words as she set out on the story of the long, tortuous path that led to her Lyme disease diagnosis, a condition accompanied by several sequelae.
Like ‘Alicia,’ who prefers to remain anonymous, many people wait months or years for an accurate diagnosis, partly because current tests give both false positive and false negative results, partly because the symptoms are similar to other diseases, and partly because health care professionals tend to turn a deaf ear to patients’ complaints.
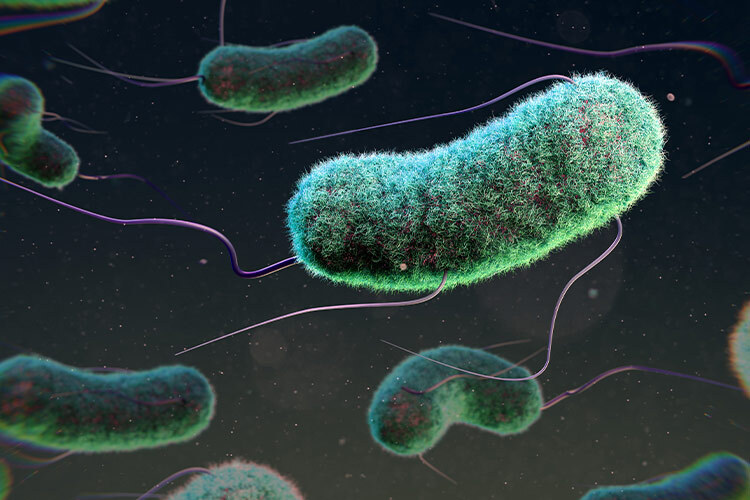
Lyme disease is caused by being infected with Borrelia bacteria, which are commonly transmitted by tick bites (genus Ixodes). Incidences of Lyme disease have risen dramatically in the United States, where it is estimated that between 300,000 and 500,000 new cases are diagnosed annually. It is also common in Europe and Canada. Around 15% of the world’s population is estimated to suffer from this disease.
What are the Symptoms?
There are a great variety of symptoms and not everyone experiences the same ones. In the first stage of Lyme disease, three to thirty days after the tick bite, symptoms typically include fever, headache, tiredness, and joint and muscle pain.
TecSalud pediatrician and infectious disease specialist César Martínez Longoria told TecScience that Lyme diagnosis requires “this set of clinical symptoms and the Erythema migrans rash in the shape of a bull’s eye at the site of the tick bite.” Martinez is referring to a rash in the shape of a bull’s eye which, if present, is an unmistakable symptom of this disease.
However, not everyone who is infected gets it. There are varying estimates of how common this welt is; some estimate that only three out of ten people get it, whereas others estimate eight out of ten. Furthermore, it is a known fact that even if present, only 6% to 20% of these welts are known to have a perfect bull’s eye shape, which makes the diagnosis confusing.
At first, Alicia’s earliest and only symptom was an itchy rash after she came into contact with a bird’s nest in Mexico City. Over the course of a couple of weeks, she visited several dermatologists, who diagnosed nervous dermatitis caused by stress. Other symptoms appeared four weeks after she got the rash. “My temperature dropped, my blood pressure dropped, I could feel my heart pounding, and I started having dizziness.”
Living a normal life started becoming difficult, especially because doctors, family members, and colleagues thought it was simply stress or a mental health issue. “Your world changes because nobody believes you, nobody takes you seriously.”
Without proper antibiotic treatment during the first month of infection, the disease can become much more serious. “The infection may shift from the blood to other places, particularly the heart, where it may cause inflammation, or the nervous system, where it may produce meningitis or inflammation of the brain; in other words, severe neurological or cardiac complications,” explains Martinez.
Furthermore, welts or rashes may become more common and move to different parts of your body, your muscles may become weak and your heartbeat irregular, pains may occur in your back, hips and legs and there may be numbness in your hands and feet, among other things. If this persists, the symptoms may become chronic and never disappear which, in turn, causes arthritis, widespread pain, and exhaustion, considerably detracting from your quality of life and often involving long periods of incapacitation.
The Challenge of Diagnosing Lyme Disease
“Diagnosis is very simple for other diseases: you suspect something, do a test, it comes back positive, and that’s it. But it’s not so easy in the case of Lyme disease. To make a diagnosis, the first thing to look at is the clinical symptoms,” says Martínez Longoria. The problem is that the symptoms of Lyme resemble those of many other conditions. “First, they could tell you you’re suffering from stress,” says ‘Alicia’ from her own experience. “Something else they bring up is your age; you tell them your knee didn’t hurt last month but now it’s really sore and they just tell you you’re getting old.”
Another important piece of information for proper diagnosis is a tick bite, which most people do not remember, especially if the symptoms do not appear immediately. “Or if you happen to live in an area where ticks are endemic; in other words, a place where ticks transmit the disease,” remarks Martinez.
Endemic Lyme disease is not believed to exist in Mexico; in other words, the cases reported are of people who went to another country and got infected there, which “makes it much less likely to suspect there could have been an infection when making a diagnosis.” However, research indicates that between 3% and 6% of the population possess antibodies to this bacterium and therefore have or have had the disease, which suggests that not all cases come from abroad.
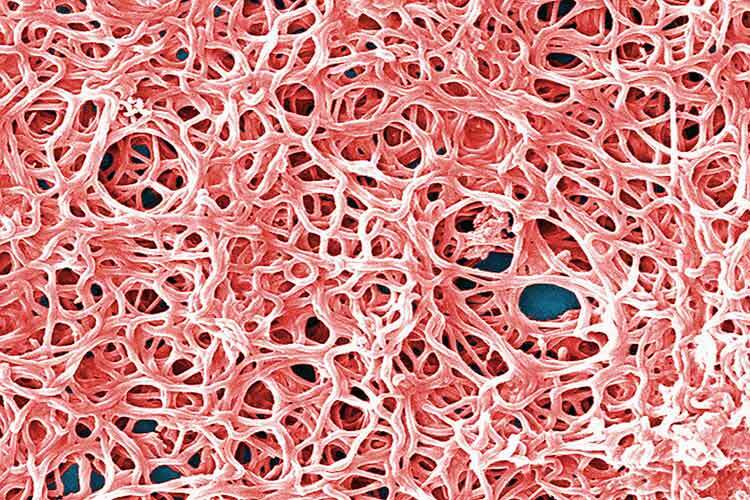
In the event of Lyme being suspected due to symptoms or clinical history, the next step is to conduct diagnostic tests. Direct tests, such as growing bacteria cultures from blood samples or a polymerase chain reaction (PCR) that detects genetic material, have major limitations for Borrelia and are rarely used as they produce confusing results.
The most commonly used diagnostic tests are indirect. These do not detect the presence of Borrelia, but rather antibodies: proteins produced by our own immune system in response to the presence of foreign bodies like bacteria. These antibodies take several days to be produced, so the test result may be negative during the first four weeks of infection, which are the most important for early treatment. It is estimated that 50-65% of these test results are false negatives; in other words, more than half of those who test negative for Lyme actually have the disease.
As Alicia’s symptoms persisted, she sought the help of other doctors and went to the UNAM Tropical Medicine Center, where she was given an important clue. “They told me I had an allergy, but they also said that if I was very, very, very, very, very, very, very unlucky, I had Lyme disease.”
She found an infectious disease specialist who prescribed tests which showed negative for Lyme, but positive for another bacterium, Bartonella, which may cause symptoms very similar to Borrelia. This diagnosis changed everything. “Suddenly, everyone believes you. I was able to submit the diagnosis to my graduate school and explain to them that I did have something and was impaired. So, I was able to take a temporary leave of absence.
‘Alicia’ was given a three-week course of antibiotics that alleviated her symptoms, but the symptoms returned at the end of the treatment. She went back on antibiotics and took them for eight months until she decided to stop and look for another option.
Co-Infections May Also Occur with Lyme
Ticks that transmit Lyme are also vectors of a variety of bacteria that cause other diseases. It is estimated that half of the patients suffering from Lyme disease have some kind of co-infection, one of the most common of which is Bartonella. The simultaneous occurrence of several symptoms of other diseases makes it more difficult to make a diagnosis.
Or, as with ‘Alicia’, only one disease may be diagnosed and treated, which makes others like Lyme invisible.
“What is most worrying about Lyme is failing to make an accurate diagnosis, taking too long to make it, and not treating the disease properly, which can lead to serious or chronic conditions. The problem of underestimating the disease or confusing it with another and not treating it properly can lead to this,” says Martínez Longoria.
‘Alicia’ found a private clinic specializing in Lyme disease in Jalisco. There, her background and symptomatology were analyzed; she was eventually diagnosed with Lyme disease and given appropriate treatment two years after the rash had appeared. “The diagnosis was like a breath of fresh air, but getting there was a nightmare.”
Alicia’s story is fairly common. According to the U.S. Lyme Disease Association, the average time taken to diagnose it in the U.S. is two years. This may vary depending on how familiar medical practitioners are with the disease, as medical judgment is one of the most relevant factors.
Martinez believes that doctors in Mexico are not sufficiently versed in this disease. “I think the main reason people don’t know about Lyme in Mexico is because there are so few cases here. As we are not considered an endemic area, we don’t really know how many there are. This prevents us from having well-defined criteria or studies available for consultation, which makes diagnosis very difficult.”
Alicia’s life has almost returned to normal since she was treated in Jalisco. Sometimes the symptoms reappear but disappear just as quickly. What does persist is a sense of mistrust, which is why she chose to remain anonymous. “It has been such a crazy experience, so strange, over such a long time, and so hard to explain. The truth is that you don’t feel like telling anyone afterwards because you think people will judge you or make fun of you.”
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx