Andrea, 26, started to feel the strain of long periods spent “alone,” without speaking to or seeing anyone during the mandatory Covid-19 lockdown in 2021. Living with her boyfriend, she would only have company at night when he returned home. Teleworking in the advertising industry, Andrea was attending weekly online therapy sessions and seeing a psychiatrist, but she still felt she was sinking into a depressive crisis.
“I cried a lot during that time, overthought everything, and thought the only way out was either sleeping all day or suicide. Then I told myself: ‘I better talk to someone.’” Andrea had previously attempted suicide, but she was aware that she didn’t want things to spiral out of control. She first reached out to close friends and family, but no one answered her. So, she quickly Googled “free psychological support Mexico City” and found a helpline.
Although Andrea already had professional support, the emergency phone counseling made a difference. She remembers talking for 45 minutes with a woman about topics unrelated to the loneliness she felt at that moment—and it helped.
In Latin America, mental health disorders surged by 20% to 40%, according to 2020 figures from the World Health Organization (WHO), reflecting the pandemic’s impact on mental health.
The pandemic also worsened depressive disorders, the most common psychiatric condition, which is one of the leading causes of disability globally and a major contributor to the global disease burden, according to a study on depression and anxiety disorders across 204 countries in 2020, driven by the pandemic.
The International Classification of Diseases defines Major Depressive Disorder (MDD) as a complex mental health condition characterized by persistently low mood, loss of interest or pleasure in activities, reduced energy, changes in appetite or weight, altered sleep patterns, difficulty concentrating, feelings of worthlessness or guilt, and recurring thoughts of death or suicide.
Mental Health and the Virtual World
By April 2021, a year and a month into the Covid-19 lockdown across most Western countries, over 60% of mental health services in Latin America were disrupted.
In Uruguay, in-person psychological and psychiatric consultations dropped by 63%, but phone assistance surged to 2,000 monthly consultations, handled by 200 psychologists. In 2020, Argentina provided over 131,000 telemedicine services, according to the Social Protection and Health Division of the Inter-American Development Bank (IDB).
The link between communication technologies and healthcare dates back to the 19th century. By 1905, the first transmission of recorded heart sounds marked the beginning of telemedicine, with the telephone already well integrated into medical practice.
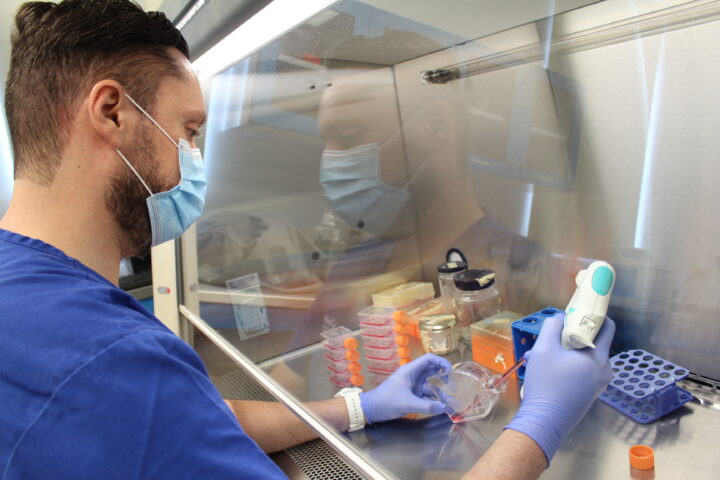
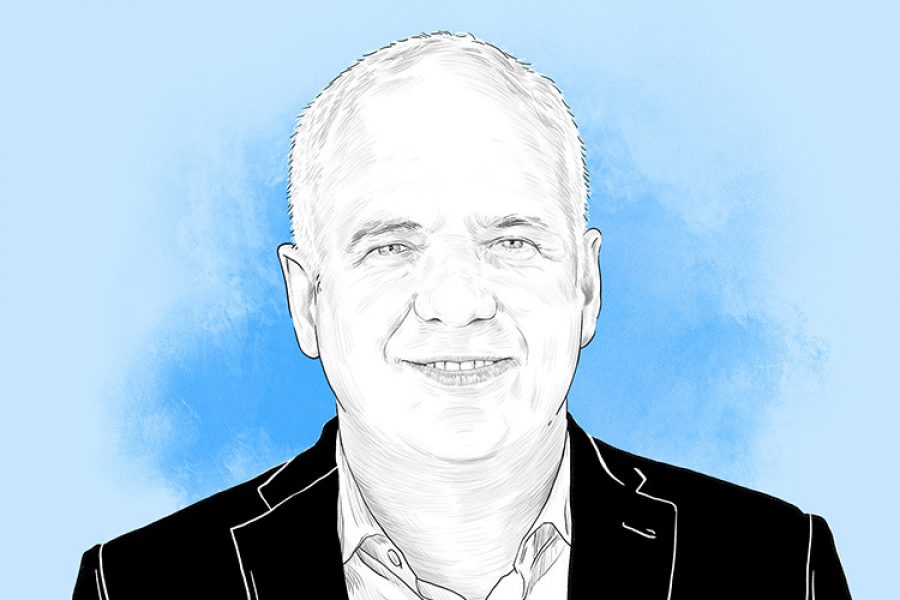
Telemedicine involves providing healthcare via virtual platforms, where professionals remotely attend to patients. This practice has been around for decades, but the pandemic caused a significant spike in its use, explains Carlos Arnaud Gil, a psychiatrist, postgrad professor at Tec de Monterrey, and director of the Advanced Psychiatry program, in an interview with TecScience.
Telemedicine Long Before Computers
Despite the persistent stigma around telemedicine for mental health—due to distrust or lack of awareness—there is clinical outcomes of telepsychiatric interventions are comparable to conventional treatment among diverse patient populations.
In the 1990s, videoconferencing and image transmission finally allowed people to connect remotely with both audio and visual contact, realizing a long-standing technological dream. As early as 1879, artist George Du Maurier envisioned this in Punch’s Almanac, illustrating a “telephonoscope” where parents viewed their distant children projected in their living room while holding a phone.
In 1879, The Lancet published a reader’s letter describing a doctor who corrected a diagnosis over the phone. A woman had called to ask whether her grandson had croup. The doctor asked her to bring the boy to the phone, listened to his cough, and then reassured her that it wasn’t serious, advising rest at home. “The anxiety subsides, and all involved are happily settled for the night,” the letter concludes.
At 30, Andrea, now discharged from virtual psychology and psychiatry services, admits she doesn’t know what would have happened if she hadn’t received assistance from the helpline during the pandemic. She had been in therapy since she was 12, but it was right before the pandemic when she began more intensive treatment with virtual psychotherapy and psychiatry.
“One thing that always kept me grounded is that I tend to build a lot of support networks. My family stood by me during that process, along with my friends and work environment. I feel like that network really helped,” she says in an interview.
For example, to meet the rising demand for mental health services during the pandemic, the Spanish municipality of Salamanca launched the free Mental Health Support Program for Coronavirus Infection (PASMICOR). This initiative broke economic barriers for vulnerable communities and significantly eased the burden on mental health services by assisting patients who no longer needed to be referred to in-person consultations.
“In our case, telemedicine interventions may explain why we didn’t record any suicides or high rates of suicidal thoughts or ideation among program participants,” states the research tracking the program’s outcomes.
Getting Online Therapy: How to Begin
For healthcare professionals, telemedicine also offers benefits, such as ensuring patient adherence to treatment and maintaining the therapeutic bond through video calls or phone conversations, even at a distance. “It’s interesting to see and get to know where the patient lives; that personal insight helps us better understand their context,” says Arnaud, who works at Zambrano Hellion Hospital.
However, Carlos takes a hybrid approach with 30% of his patients, alternating between in-person and online consultations, preferring to conduct at least one in-person session, with the rest held remotely.
“Anyone who knows how to use a computer or phone can take online therapy. I have patients as young as 15 and as old as 80, connecting from home,” says the psychiatrist.
When choosing this modality, Arnaud advises patients to always verify the credentials and licenses of the professionals they contact.
Online therapy offers various benefits, particularly for seniors and people with disabilities. It also provides greater privacy for many, making the therapeutic experience less intimidating, more convenient, and time-saving by eliminating the need for travel. However, challenges remain.
Regarding virtual mental health care, studies indicate persistent issues such as ensuring connectivity nationwide, safeguarding patient privacy during sessions, and allowing patients the freedom to express themselves, notes Arnaud. While less common, prescribing certain medications remains a challenge since some still require an in-person prescription. But these gaps are gradually closing.
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx