Lung transplants can mean a new life for those who have conditions that make breathing difficult or impaired. However, only around 20% of the total number of lungs donated each year are viable globally. Fortunately, there is an innovative procedure known as ex vivo perfusion, which could help to achieve more successful transplants.
There are millions of people across the world living with diseases that affect their lungs. These include COPD (chronic obstructive pulmonary disease), pulmonary emphysema, pulmonary fibrosis, cystic fibrosis, and pulmonary hypertension. For these people, depending on the severity of their disease, just breathing can feel like an exhausting activity, which greatly reduces their quality of life.
“Nowadays, there are people who can’t stand up because they feel like they’re drowning,” says Felipe Undurraga, Head of Lung Transplantation at the Las Condes Clinic in Chile, in an interview with TecScience.
In cases where medications or other treatments have already been tried without success, lung transplants may be the best or only solution. The procedure involves replacing this pair of organs with healthy ones, which are generally donated by deceased people.
As with most transplants, there is a global shortage of donors and waiting lists are often long. Sometimes, patients die waiting to receive one.
To complicate the situation even more, around 80% of the lungs that do get donated are discarded. This is due, in part, to logistical problems during their removal, but also because not everyone’s lungs are healthy enough to donate.
Certain factors, such as smoking, living in polluted environments, or having mild respiratory diseases, could mean that they cannot be used in a transplant.
What is perfusion?
With this problem in mind, a revolutionary method for evaluating the lungs and hearts of potential donors was attempted on an animal model in the 1970s, creating a system that would keep them alive long enough to know if they were viable before surgery.
This method, which can also be used for other organs, was called ex vivo perfusion.
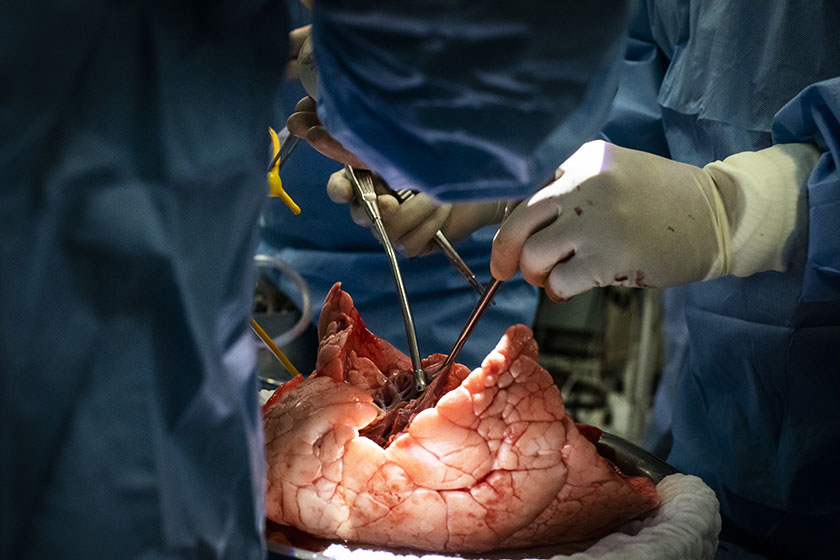
In essence, the procedure involves removing the donated organ, placing it in a polycarbonate dome, and connecting it to a system where it is ventilated and perfused with a solution that mimics blood. This ensures that the tissue remains alive long enough for surgeons to evaluate it.

In 2001, a group of scientists and surgeons from the University of Lund, Sweden, performed the first successful lung transplant using ex vivo perfusion. In 2008, a group of scientists from the University of Toronto perfected the technique and created an improved protocol, which is the one most widely used today.
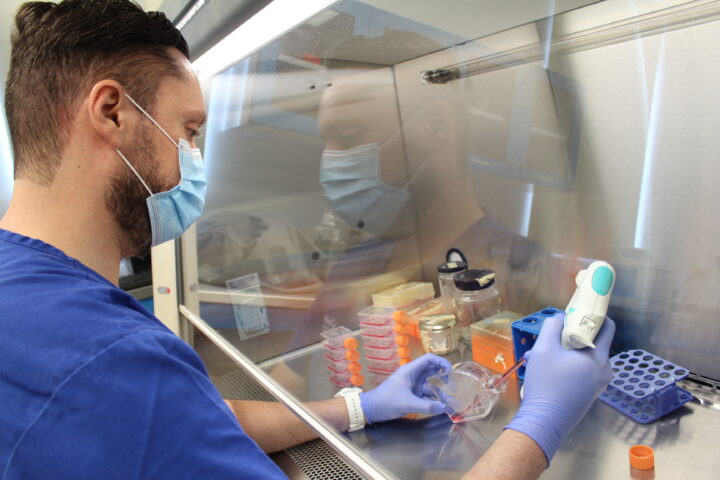
During ex vivo lung perfusion, the lungs are removed from the donor. On the operating table, one specialized plastic cannula is connected to the left auricle and another to the pulmonary artery. The lungs are then transferred to the dome under sterile conditions.
Once there, the part of the trachea that sits between the lungs is connected to a ventilator like the ones used in intensive care units. Via the left auricle and the pulmonary artery, the lungs are also connected to a system that consists of a reservoir containing the perfusate, a centrifugal pump that pumps the solution, a membrane oxygenator, and a heat exchanger.
The circuit begins in the left auricle and the flow returns through the pulmonary artery.
An improved protocol and the Steen solution
Currently, this protocol enables surgeons to not only assess the viability of these organs but also to improve them and recover those that were going to be discarded.
According to Undurraga, who was the first to perform the technique in Latin America, “the aim is to achieve better lungs than those given to us by nature.”
Part of the procedure’s success is the Steen solution. This was developed by Swedish doctor Stig Steen, and works like improved artificial blood, which also has an antioxidant effect.
Its ingredients include human serum albumin, which prevents inflammation, Dextran 40, which protects the outer layer of the lungs and promotes circulation, extra-cellular electrolytes, which prevent spasms and reduce oxidative stress, and glucose, which provides energy.
Antibiotics and medications are often added to the solution to kill harmful bacteria and other microorganisms in the lungs.

Tec de Monterrey joins the challenge
Thanks to ex vivo lung perfusion, the countries performing it have seen an increase in viable lungs, as well as a better response from the bodies of the patients who received the transplant.
However, its complexity means it is only performed in a few places in the world, such as Sweden, Canada, the Netherlands, Japan, Italy, Germany, and the United Kingdom. In Latin America, it is only performed in Chile.
With the aim of bringing the technique to Mexico, Tecnológico de Monterrey hosted the Ex Vivo Lung Perfusion Workshop at the School of Medicine and Health Sciences on January 27 and 28, 2023.
In a series of talks from expert panelists on the topic, the need to bring it to the country was discussed and students and doctors were taught how to perform it. On the second day, an animal model demonstration was given to start training staff, students, and surgeons.
The idea is for TecSalud hospitals to eventually become centers for training and organ preservation, in order to send improved lungs to the rest of the country and other parts of Latin America.
“At times, we think that certain technologies aren’t attainable,” said René Gómez Gutiérrez, director of the ECMO and Advanced Cardiopulmonary Support Therapies Program at TecSalud Hospitals, in an interview with TecScience. “But Tecnológico de Monterrey has the education and research infrastructure and all the human talent to do it.”