Phototherapy refers to a treatment induced by light or radiant energy. This innovative vision-saving procedure has emerged as a near-miraculous treatment, reshaping the trajectory of corneal diseases such as keratoconus. This condition is a malformation of the cornea and is the most common cause of corneal transplants, especially in young people.
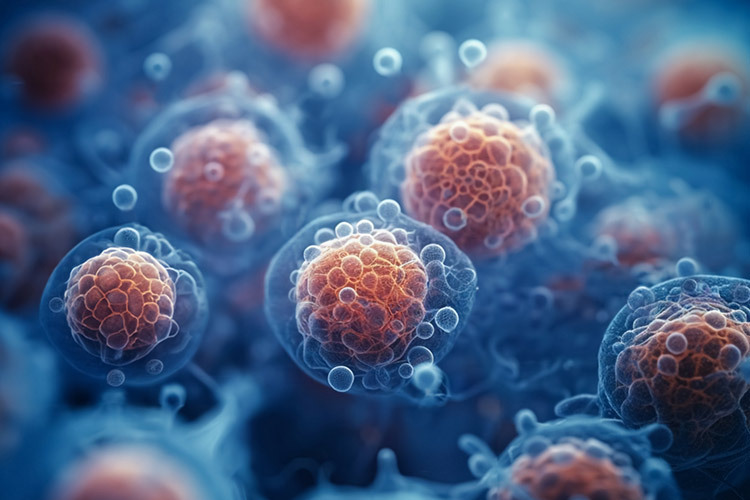
The cornea serves as a crucial shield for the eye, safeguarding it against both trauma and infections. Composed of transparent, avascular connective tissue, it boasts an average central thickness of 540 micrometers, or 540 thousandths of a millimeter. To withstand the various stresses exerted upon it, the cornea maintains a delicate and complex balance of stiffness, strength, extensibility, and overall hardness.
Keratoconus is a bilateral, predominantly asymmetrical, progressive condition characterized by the thinning and protrusion of the cornea, resulting in irregular astigmatism. Left untreated, it can lead to blindness due to central scarring of the eye.
This condition, also known as a cone-shaped and thinned cornea, can be congenital but typically emerges during puberty or shortly thereafter. It tends to progress for six to eight years and then stabilizes, although it can worsen at any time in life.
How Does Phototherapy Work?
The only treatment demonstrated to effectively halt the progression of keratoconus is Corneal Collagen Cross-Linking (CXL).
CXL, or “Cross-Linking,” is a specific medical procedure used to strengthen the collagen in the cornea. This minimally invasive procedure prevents the progression of corneal ectasia, such as keratoconus, and post-LASIK ectasia, a surgery used to reshape the cornea.
Surgeons have used collagen fiber cross-linking for the last 20 years to stop keratoconus progression. Evidence shows that the cornea improves topographically and functionally after CXL.
In the late 1990s, researchers at the University of Dresden developed the foundations of current corneal collagen CXL techniques. They used ultraviolet light to induce cross-linking of collagen fibers in riboflavin-soaked pig and rabbit corneas through oxidation. The resulting corneas were stronger and more resilient.
Corneal Collagen Cross-Linking (CXL) relies on three primary components: a photosensitizer, an ultraviolet light source, and the ensuing photochemical reaction. Photosensitizers absorb light energy and chemically alter another molecule.
Riboflavin, a commonly used photosensitizer in CXL, is topically applied to the corneal stroma and is considered safe for systemic use. When combined with UV-A light during CXL, riboflavin alters the biomechanical properties of corneal collagen.
Treating Keratoconus
Keratoconus stands as one of the prevailing reasons for corneal transplants globally. As mentioned above, typically emerging during adolescence, its progression extends into the third or fourth decade of life.
Our research group in advanced therapies for visual sciences found that the prevalence of keratoconus in adolescents seeking ophthalmologic consultation was 1.8%, affecting 66.6% of females and 33.3% of males, with an average age of 16.1 years. The most associated refractive error was astigmatism (44.4%); bilateral cases accounted for 88.8%.
Before CXL techniques, the standard of care for keratoconus changed very little over the years. Due to its progressive nature, about 10% to 20% of patients eventually required some form of keratoplasty, also known as a corneal transplant.
The natural process of collagen fibrils forming robust chemical bonds with neighboring fibrils, referred to as cross-linking or CXL, typically happens with aging. This inherent collagen cross-linking may elucidate why corneal ectasia advances more rapidly during adolescence or early adulthood but tends to plateau after middle age.
Research at TecSalud
Our group conducted research evaluating the visual and topographic outcomes of two protocols of a new CXL treatment modality, accelerated by pulsed light (A-CXL), in young adult patients with progressive keratoconus. Both protocols proved effective and safe for achieving topographic stabilization or improvement in over 85% of eyes at 12 months post-treatment.
The treatment algorithm for keratoconus and corneal ectasia has undergone significant transformation with the introduction of CXL.
Early detection of the disease is now more critical than ever. Previously, doctors had to inform patients that their condition would worsen over time and that keratoplasty was inevitable. Today, CXL can help prevent these limitations, enabling patients to function optimally.
In a comparative study by our group, pulsed CXL results for pediatric and adult keratoconus showed that, after one year of follow-up, pulsed ACXL is equally safe and effective in halting disease progression in both adults and children. Visual, refractive, and topographic outcomes improved in both groups.
Recent scientific advances have enabled us to identify these patients timely, allowing for early treatment during adolescence.
CXL has become the standard of care due to the benefits of early detection and timely treatment, as well as subsequent visual rehabilitation with intrastromal rings (intracorneal implants placed inside the eye) and scleral contact lenses, which support the cornea without resting on it, avoiding irregularities and improving vision.
The current frontier is understanding the interaction between environmental, biochemical, behavioral, and genetic factors in keratoconus development. Utilizing advanced technology to assess the disease at genetic and cellular levels is imperative for uncovering its genetic origins.
References
This article is based on the scientific publications by professors and students in the Advanced Therapies in Ophthalmology and Visual Sciences Research Group.
- Importance and use of corneal biomechanics and its diagnostic utility. Arturo Ramirez-Miranda, Simran Mangwani-Mordani, José Y Arteaga-Rivera, Renato Ambrosio Jr, Alejandro Navas, Enrique O Graue-Hernandez, Jorge E Valdez-Garcia. Surgery and Surgeons 91 (6), 848-857. 2024
- Evaluation of topographic indices in Hispanic patients with Keratoconus and Keratoconus suspects. LL Franco, P Lopez, JC Hernandez, JE Valdez. Investigative Ophthalmology & Visual Science 56 (7), 1631-1631. 2015.
- Corneal topography index in patients with suspected keratoconus. Jorge E. Valdez-Garcia, Alfonso Luis Gonzalez Gonzalez, Francisco Durán Iñiguez, Andres Madero Frech. Avances Journal. September 2005
- Central corneal thickness and minimum corneal thickness difference analysis in keratoconus patients based on optical coherence tomography. MGG Quintanilla, LGV Valdez, J Zavala, JE Valdez. Investigative Ophthalmology & Visual Science 61 (7), 2594-2594. 2020
- Prevalence of keratoconus in an adolescent population. JE Valdez-García, R Sepúlveda, JJ Salazar-Martínez, JF Lozano-Ramírez. Mexican Journal of Ophthalmology 88 (3), 95-98. 2014
- Complications of Ferrara intrastromal rings utilization in keratoconus treatment. Jorge Eugenio Valdez García, Francisco Segura Lozano, Angelina Espino-Barros Palau, Montserrat Guraieb Trueba, Adriana Hernández López, Jorge Carlos López Morán, César David García Garza. Mexican Journal of Ophthalmology 81 (4), 205-208. 2007
- Correlation between corneal stromal demarcation line depth and topographic outcomes after two pulsed-light-accelerated crosslinking protocols. Julio C Hernandez-Camarena, Enrique O Graue-Hernandez, Denise Loya-García, Raul E Ruiz-Lozano, Jorge E Valdez-García. Clinical Ophthalmology, 1665-1673. 2019
- Outcomes of accelerated corneal cross-linking for pediatric and adult keratoconus: a comparative study. Andres Bustamante-Arias, Julio C Hernandez-Camarena, Alejandro Rodriguez-Garcia, Raul E Ruiz-Lozano, Luis A Rodriguez-Gutierrez, Jorge E Valdez-Garcia International Ophthalmology 44 (1), 145. 2024
- Scleral lenses for the management of corneal irregularities. Visual and aberrometric outcomes in Mexico. Denise Loya, Gustavo Ortiz-Morales, Monica Herrera-Rodriguez, Julio Hernandez-Camarena, Guillermo Garcia de la Rosa, Jorge Eugenio Valdez-Garcia. Investigative Ophthalmology & Visual Science 62 (8), 678-678. 2021.
- Genetic alterations associated with keratoconus, bioinformatic research and a functional analysis. Manuel Antonio Salinas-Lugo, Manuel Emiliano Quiroga-Garza, Daniel Bastán-Fabián, Jesus Enrique Arreola, Raul Eduardo Ruiz, Maricruz Sepulveda-Villegas, Victor Treviño, Julio Cesar Hernandez-Camarena, Jorge Eugenio Valdez-Garcia. Investigative Ophthalmology & Visual Science 63 (7), 2382–A0185-2382–A0185. 2022
Author
Jorge E. Valdez-García. Subspecialist Ophthalmologist, Master in Medical Sciences, and Doctor in Surgical Research, Professor and Head of the Cornea and Refractive Surgery Service at the Institute of Ophthalmology and Visual Sciences of Zambrano Hellion Medical Center, TecSalud. He leads the Innovative Therapies in Ophthalmology and Visual Sciences Research Group (GIEE) at the School of Medicine and Health Sciences, Tecnológico de Monterrey. He is a member of the National System of Researchers, Level 2, and a full member of the Mexican Academy of Surgery.