On platforms like TikTok, content related to weight loss drugs and procedures has surged, often explained by non-health professionals, which can lead to misinformation. Among the trending topics is bariatric surgery. But what exactly is it, and who should consider it?
Ricardo Cuéllar Tamez, a bariatric surgeon at TecSalud, explains in an interview with TecScience that bariatric surgeries, such as gastric sleeve and gastric bypass, are statistically proven to be the gold standard for long-term weight loss. However, these procedures are primarily for cases of obesity, particularly grade II and III, which must be evaluated by health experts.
According to the World Health Organization (WHO), obesity is defined as excessive fat accumulation that poses health risks, such as type 2 diabetes, heart disease, bone and reproductive health issues, and an increased risk of certain cancers. It also affects quality of life, impacting sleep and mobility.
To determine if we are overweight or obese, one key marker is the Body Mass Index (BMI), calculated by dividing our weight by our height squared. For example, if I am 1.60 meters tall and weigh 55 kilograms (55/1.60×1.60), my BMI would be 21.4. If I gain weight to 80 kg, it results in a BMI of 31.2; at 110 kg, it’s 42.9, and at 170 kg, it rises to 66.4.
The WHO classifies a BMI of 18.5 to 24.9 as normal, 25 to 29.9 as overweight, and obesity into three grades: grade I (BMI 30-34.9), grade II (BMI 35-39.9), and grade III (BMI over 40). Many bariatric experts add a grade IV for BMIs over 50, known as extreme obesity or super obesity.
What is Bariatric Surgery and Who is it For?
Cuéllar Tamez notes that while BMI alone doesn’t determine overweight or obesity, it provides a guideline. If your BMI indicates a health risk, it’s ideal to make lifestyle changes, consult a nutritionist, and increase physical activity. But what if these adjustments don’t lead to weight loss?
The Mexican Social Security Institute (IMSS) guidelines for the surgical treatment of adult obesity, updated in 2018, defines bariatric surgery as a set of surgical procedures indicated primarily when medical treatment (diet, exercise, lifestyle changes, pharmacological treatment, behavioral changes, and psychological support) fails to achieve sustained weight loss.
This is where bariatric surgeons come in. They can assess if you have any metabolic conditions hindering weight loss, provide medications, and determine if you are a candidate for bariatric surgery in certain cases of obesity.
“Patients need thorough evaluation,” says Cuéllar Tamez. “Bariatric surgery is recommended starting at grade II obesity with metabolic diseases. New global standards now even consider grade I obesity, but we must choose the best techniques for each case.”
For instance, “gastric sleeve is generally recommended for grade I or II obesity, while bypass might be needed for grade III,” he explains, noting that the best treatment depends on each patient’s medical history.
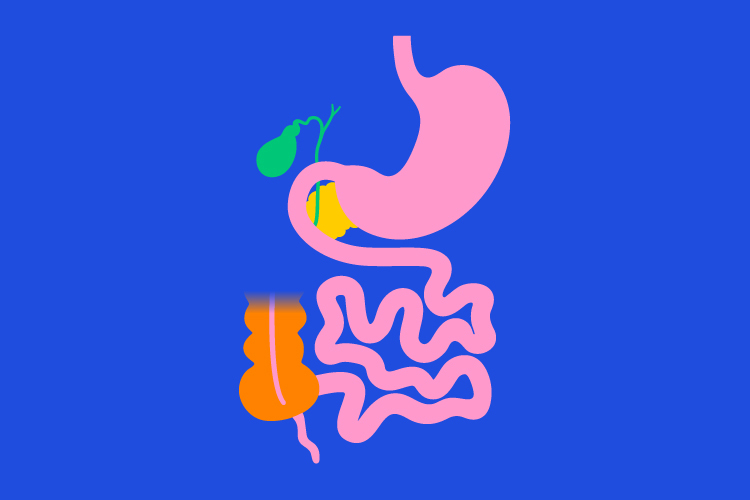
Common Bariatric Surgeries
Cuéllar Tamez mentions that the gastric sleeve is the most common procedure worldwide, accounting for 70% of bariatric surgeries, recommended for type I and II obesity. Gastric bypass is indicated for grade III and IV obesity.
The gastric sleeve procedure reduces stomach size. “Instead of having the capacity of a football, it’s reduced to the size of a banana, with about 70% of the stomach removed,” says Cuéllar.
This surgery is mainly recommended for patients with grade II obesity and chronic degenerative diseases like hypertension and diabetes. However, the expert adds that “the standard is changing, and gastric sleeve can also help grade I obesity patients with conditions like insulin resistance, polycystic ovary syndrome, and metabolic diseases.”
Gastric bypass, on the other hand, is both restrictive and malabsorptive, reducing stomach size and connecting it to the small intestine. It’s typically for “heavier patients with metabolic diseases like diabetes or dyslipidemia (high cholesterol and triglycerides).”
Benefits and Risks of Bariatric Surgery
A June 2024 study in Nature reveals that individuals who underwent bariatric surgery 15 years ago now experience improved health and mood, and fewer obesity-related and social interaction issues compared to those who opted for non-surgical treatments.
Another study in the European Heart Journal in 2022 found that “bariatric surgery is associated with reduced cardiovascular mortality and a lower incidence of various cardiovascular diseases in obese patients.”
Cuéllar Tamez notes that “bariatric surgery improves diabetes cases by 83%, putting it in remission because long-term weight loss decreases the burden on the pancreas. Even in insulin resistance cases, it can prevent progression to diabetes.”
For BMIs over 35 (grade II obesity), other comorbidities like hypertension, fatty liver, and sleep apnea also improve, with sleep apnea reducing by up to 90%. In grade III obesity patients, “quality of life improves by 95%, and mortality reduces over five years due to lowered cardiovascular risk,” says the specialist.
Regarding risks, Cuéllar Tamez states that “bariatric surgery today should be comparable to gallbladder surgery or a cesarean in terms of complication rates, very low, provided it’s done in a center where it’s routinely performed.” This ensures experienced bariatric surgeons, nurses, and anesthesiologists handle the procedures.
“These are minimally invasive laparoscopic techniques; patients recover in seven days and can walk out as the incisions are small, and recovery is swift,” explains Cuéllar.
However, he warns, “I tell patients it’s not a magic wand. It’s a powerful tool but not a game. It requires a commitment to dietary changes, physical activity, and supplementation.”
This last point is crucial because gastric bypass patients often face “malabsorption of certain nutrients, micronutrients, and vitamins like calcium, iron, and vitamin D, necessitating lifelong supplementation,” says Cuéllar.
In gastric sleeve cases, “there are no issues with vitamin and mineral deficiencies, but all patients are advised to supplement with iron for at least 3, 4, or 5 years,” emphasizes the surgeon.
Who Are Bariatric Surgery Specialists?
Bariatric surgeons specialize in these surgeries, but it’s essential they have a multidisciplinary team, including a nutritionist, psychologist, and internist, to provide comprehensive evaluation and follow-up for the patient’s conditions.
Both the nutritionist and psychologist must be experts in bariatric patient care. Cuéllar notes that creating a plan for a patient with an average BMI seeking healthier eating or losing a few pounds differs significantly from managing someone with grade II or III obesity undergoing bariatric surgery.
The psychologist familiar with bariatric cases understands the challenges patients face post-surgery, many of which are positive, but they must be prepared to overcome them, explains the specialist.
This multidisciplinary team can better assess candidates for surgery and offer alternatives for those who don’t qualify. For example, some patients need stabilization before surgery due to uncontrolled conditions like diabetes.
“I tell some patients, ‘I need to control your condition before surgery to ensure your safety. If you have uncontrolled diabetes or hypertension, there’s a higher risk.’ That’s why an internist is part of the team to manage such cases,” says Cuéllar.
Is it Difficult to Access Bariatric Surgery in Mexico?
The answer is yes, but with limitations. Cuéllar Tamez notes that “bariatric surgery is accessible to only 1% of the population because it’s expensive in the private sector, and public health programs are insufficient to cover the need. Therefore, the number of patients we serve is low, although many more could benefit.”
How many could benefit? In Mexico, 75.2% of the adult population (20 years and older) is overweight or obese, according to the National Health and Nutrition Survey (Ensanut). These conditions have an economic impact equivalent to 2.1% of the GDP due to associated chronic diseases’ healthcare costs.
For example, “90% of type 2 diabetes cases in the country are attributed to overweight and obesity,” according to the IMSS obesity treatment guide. Reducing the BMI of these patients could decrease comorbidities and healthcare expenses, making bariatric surgery a valuable tool.
In November 2020, the Senate approved changes to the General Health Law, allowing all public institutions within the National Health System to integrate bariatric surgery as a treatment for obesity and its comorbidities. However, it’s unclear how many have accessed this service since then.
A 2022 government website report states that between 100 and 150 bariatric surgeries are performed annually at the Obesity Clinic of the “Manuel Gea González” General Hospital. Still, national data on such procedures in public institutions is scarce.
What to Consider Before Bariatric Surgery
If you have access to these treatments privately, Cuéllar recommends finding a reputable surgeon (check their credentials, certifications, and professional experience). “The most important factor for long-term success is having a multidisciplinary team supporting you throughout the process, not just during surgery.”
The expert emphasizes that your surgeon should order preoperative tests to understand your health status before surgery. “Some patients undergo surgery with just a basic blood test, which isn’t enough.”
“You need evaluations from a psychologist, nutritionist, and the surgeon to see if you are a candidate. I request an ultrasound, thyroid check, X-ray, and electrocardiogram to ensure complications are less than 1% and mortality is 0%,” adds Cuéllar.
It’s crucial that they also explain the differences between both techniques and help you determine which is best for you: “Some patients come to me saying, ‘I want a gastric sleeve,’ and I tell them, ‘You’re not a candidate because you have acid reflux or your BMI isn’t high enough. This surgery is too much for you, and I won’t perform it.’ Instead, I recommend a treatment that is better suited for their health condition and will benefit them more in the long run.”
Which is the Post Bariatric Surgery Care That I Should Follow?
According to Cuéllar Tamez, it’s a myth to say that bariatric surgery is the “easy way out” because “patients need to commit, and it’s not simple. You have to start like a baby. The post-bariatric surgery diet involves two weeks of liquids, two weeks of purees, then slowly introducing solids. By three months, the patient is eating solid food, and this process is complex.”
However, the specialist adds: “I tell my patients that they need to be ready for a radical change because we’re starting from scratch. It’s a clean slate, a new opportunity to do things right. But if you have doubts, it’s better to have the surgery when you’re truly ready because the changes are amazing, and the more effort the patient puts in, the better the results.”
“By putting in effort, I mean sticking to the diet, being more physically active, and taking supplements. Those three things. But supplementation isn’t as complicated or expensive as people think. I prescribe a special bariatric multivitamin that’s not very costly—you just take one pill a day, and it lasts for three months,” he notes.
Keep in mind that you’ll need follow-up for five years because “bariatric surgery has a honeymoon period —the first two years— when the patient might take great care and do well, but weight regain can occur. That’s where education comes in. We help them understand better how and what to eat, but it’s also a commitment for them to change their lifestyle and be more physically active,” says the specialist.
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx