In June 2021, Carlos Colunga, a pediatric surgeon in Monterrey, contracted COVID-19. At 33 years old, he was in good health and his illness was very mild. Three weeks later, when he had already tested negative for SARS-CoV-2, a loud sound invaded his ears. The tinnitus he suffered only gave him relief when he was under the shower because the noise of the falling water was louder than the hiss he heard.
A week later his symptoms worsened. Traveling a distance, which was not difficult for him before, made him exhausted, in addition, he felt strong palpitations in his chest and couldn’t breathe. Desperate, he started looking for help. He had to consult more than five specialists to find one who finally diagnosed a probable cause: the poorly understood Long COVID or persistent COVID.
“It was a very stressful and exhausting process, never in my life had I cried so much,” says Carlos in an interview with TecScience.
What is Long COVID?
What Carlos Colunga didn’t know is that he wasn’t alone, his case is one in millions.
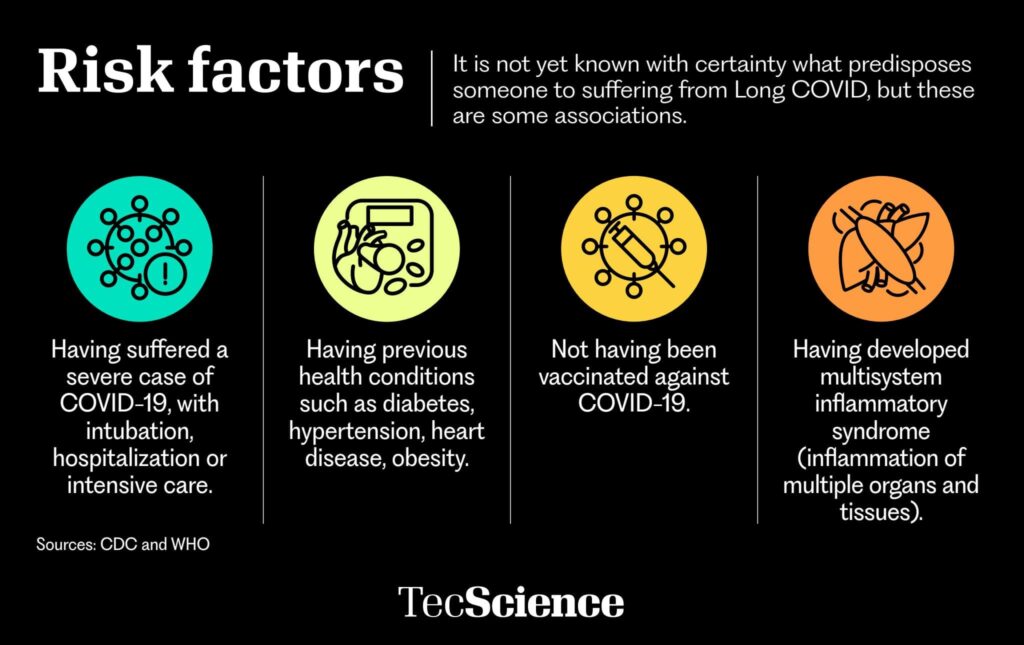
There is still no consensus in the scientific community on what Long COVID is –also known as persistent COVID or post-acute COVID-19– nor a test or tool to diagnose it.
Nevertheless, the World Health Organization (WHO) defines it as a set of prolonged symptoms that some people show after getting infected with COVID. A review published in the journal Nature estimates that around 65 million people around the world suffer from it, out of a total of 670 million registered cases of SARS-CoV-2, that is, 10% of the population that was infected.
In Mexico, data is limited. An analysis of 50 cases, carried out by Hospital Ángeles Puebla in 2020, found that 84% of them presented persistent symptoms after recovering from the initial illness.
“There are more questions than answers,” says Paola Reynoso Lobo, Leader of Public Health Projects and professor at the School of Medicine and Health Sciences at Tecnológico de Monterrey.
WHO has created a list of more than 200 symptoms associated with this condition.
“The most common ones are fatigue, shortness of breath, mental fog, palpitations, and headaches,” explains Reynoso. Others include loss of taste and smell, persistent cough, diarrhea, trouble sleeping, dizziness, muscle pain, and rashes.
Neurological and emotional symptoms
Sara’s experience –a 68 years old patient who asked to give her a pseudonym– was in pain, sad, and frustrated. “I started having panic attacks, feeling like going out on the streets to scream,” she recalls.
In March 2021, Sara was infected with COVID-19. Like Carlos, the initial illness was mild, with a sore throat, runny nose, and fever. She recovered and within two weeks she began to experience headaches so severe that they woke her up at nights. In addition, she had fatigue, anxiety, and depression.
The outlook did not look good for Sara. “I had a lot of anguish, I hardly slept,” she says.
The most difficult symptoms to live with and understand for those with Long COVID are those related to our brains and emotions. Many report memory problems, insomnia, difficulty concentrating, balance problems, dizziness, light sensitivity, slurred speech, anxiety, and depression.
According to Héctor Ramón Martínez Rodríguez, researcher and neurologist, director of the Institute of Neurology and Neurosurgery at the Zambrano Hellion Hospital, up to “82% of patients hospitalized for COVID-19 show neurological and neuropsychiatric symptoms, during the event and months after.”
Among these ailments, there is brain fog. This is characterized by a state of confusion, forgetfulness, lack of concentration, and no mental clarity. Many times, it can feel like the effects of stress or lack of sleep.
Scientific research has found that up to 40% of people who experience Long COVID have at least one of the symptoms of brain fog at some point.
For those who have suffered it, the frustration can be even greater as people around them may think they are lying or making it up, simply because they don’t want to go to work.
Some patients have reported having health professionals dismiss them. Experts Martínez Rodríguez and Reynoso Lobo explain that brain fog can be incapacitating, and it would be unusual for people to fake it.
The reasons why Long COVID can cause these emotions are still unknown. However, neurologist Héctor Martínez suggests that one of the causes could be due to the direct invasion of the SARS-CoV-2 virus in the brain.

A social media support group
In 2021, when more Long COVID cases were being reported, at TecSalud’s Zambrano Helión Hospital, a team led by Paola Reynoso began to investigate what could be done to help.
They found that many people who believed they were living with Long COVID had begun organizing themselves through social media to share scientific information about the condition, and give each other advice and encouragement.
They discovered that a common denominator in these groups was that people felt little understood by health professionals. “They couldn’t find answers and were even being invalidated, with them saying that −surely− it was some other condition or that perhaps they were making it up,” says Reynoso Lobo.
To contribute, the researcher and her team created a virtual support group, in which they offer sessions with health experts, such as neurologists, cardiologists, psychologists, nutritionists, psychiatrists, otolaryngologist, or infectologists.
The idea was to create a space where people could feel accompanied and obtain information and recommendations based on scientific evidence. Restorative yoga or meditation classes have also been taught in the sessions. The group is on Facebook and is open to the public.
For Carlos Colunga, the help the group has given him is invaluable. “I think that what it contributes the most is that it’s a space where people realize they aren’t alone,” he reflects.
Personalized treatments
It is difficult to know for sure that someone has Long COVID. Because this is a new and unknown condition, doctors are still learning and are sometimes afraid to diagnose their patients, for fear of losing their good reputation or mistakenly diagnosing someone.
Fortunately, more and more experts are now open to the idea. The treatment given to patients depends on the symptoms they present. “There is no textbook approach, rather, depending on what the patient is showing, an individualized treatment plan is made,” explains Reynoso Lobo.
Martínez Rodríguez and Reynoso Lobo advise that people who believe they might have Long COVID should approach their family doctor for an initial evaluation so they can refer them to a specialist, depending on the severity of their symptoms.
Carlos and Sara both had personalized treatments. He was given a serie of medications and Sara began taking therapy, exercising, and meditating.
Carlos has less and less tinnitus and fatigue, while Sara has regained her mental health and her headaches have been significantly reduced. “I think that we are all going to get better,” says Sara.