Billions of people around the world have received the Pfizer or Moderna COVID-19 vaccines. The rapid development of these vaccines changed the course of the pandemic, providing protection against the SARS-CoV-2 virus.
But these vaccines would not have been possible it if weren’t for the pioneering work of this year’s winners of the Nobel Prize in physiology or medicine decades earlier.
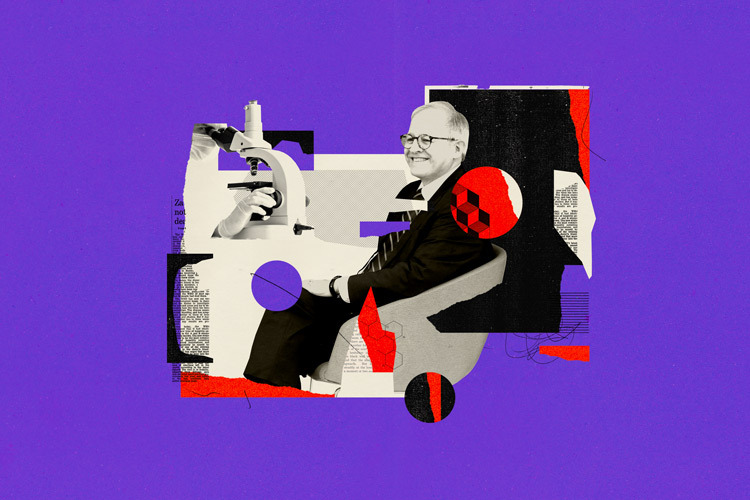
Winners of the 2023 Nobel Prize in Medicine
Katalin Karikó and Drew Weissman, researchers from the University of Pennsylvania, have been given the prestigious award for their discoveries in mRNA biology. The pair (who met in line for a photocopier) were the first to discover a way of modifying mRNA that allowed it to successfully be delivered to cells and replicated by them.
Their discovery was not only integral to COVID-19 vaccine development, but may also lead to the development of many other therapies – such as vaccines for cancer.
Karikó is a Hungarian biochemist and Weissman an American physician scientist. The two began working together in 1985 when Karikó was a postdoctoral researcher at the University of Pennsylvania, where Weissman was already working as an immunologist. They had a shared interest in how mRNA could be used to make new therapies.
What is mRNA?
Messenger RNA (better known as mRNA) is an essential molecule to life. It’s made in the body from our very own DNA in a process called translation. DNA is our special encoded handbook of instructions for manufacturing proteins, which are the building blocks for material in the body.
Our mRNA copies and carries these genetic instructions from our DNA to our cells. The cells then make whatever protein they’ve been instructed to, such as haemoglobin for helping red blood cells carry oxygen around the body.
Karikó and Weissman thought that if it was possible to commandeer this process, mRNA could be used to instruct cells to essentially make their own cures. But at the time they started working together, attempts by other researchers to do this had been successful.
The researchers faced two major challenges as they began their work. The first was being able to prevent the host from mounting an immune response against the modified mRNA. The second was being able to deliver the mRNA into the host safely without it degrading.
To understand how they overcame the first barrier, it’s important to understand mRNA’s structure. Normally, mRNA molecules contain four types of smaller molecules known as bases (nucleosides): A (adenine), U (uridine), G (guanine), and C (cytosine). Different sequences of these bases can be strung together to produce the basis of an mRNA molecule.
In early experiments, Karikó and Weismann found that injecting normal mRNA molecules into mice led to an immune response. This meant the mouse’s immune system saw the new mRNA as an invading pathogen and the immune cells would destroy it, instead of replicating it.
So, the researchers modified the U nucleoside to create a pseudouridine, a chemical compound which stabilises RNA’s structure. When they repeated their experiment with the modified mRNA, the mice exhibited no immune response.
But Karikó and Weismann still faced the second challenge of being able to deliver the bespoke mRNA without it degrading.
The use of nanoparticles
They decided to use lipids (a nanoparticle) to deliver it. These fatty chemical compounds are an essential part of the cell membrane, controlling what enters and leaves the cell. Specially created lipids allowed the mRNA molecules to be delivered without being degraded or broken down by the immune system.
Karikó and Weissman’s research had successfully eliminated the obstacles that had previously stood in the way of using mRNA clinically. Being able to instruct the body to replicate virtually any harmless protein could have potential for treating a range of diseases and even protect against viral infections.
When their research was first published, it didn’t garner much attention. But in 2011, two biotech companies – Moderna and BioNTech – took notice and began research into mRNA medicines.
It’s no wonder why. Traditional vaccine production methods are time consuming, expensive and don’t work for every vaccine. But Karikó and Weissman’s work showed that synthetic mRNA could be made at a large scale.
Researchers had already been working on developing mRNA vaccines before the pandemic, such as a vaccine for Ebola that didn’t receive much commercial interest. But in 2020, when COVID-19 began spreading around the globe, vaccines were needed quickly to offer protection.
Using the foundational work of Karikó and Weissman, scientists developed a bespoke mRNA sequence which mimicked the spike protein (which allows the virus to enter our cells). This produced a harmless COVID particle which our cells then replicated, allowing our bodies to protect us from severe COVID infections when it encountered the real virus.
Karikó and Weissman’s discoveries years earlier were critical in making the COVID-19 mRNA vaccines possible. But these aren’t the only ways their work could be applied.
Researchers are now hoping to developing mRNA vaccines from diseases such as HIV and Zika virus. Studies have also shown mRNA vaccines might be useful in treating certain types of cancer.