When we read the word design, we almost always think of industrial or graphic design, without imagining that it can also be used to design healthcare systems, not only to ensure they function well, but also to improve in the face of new challenges.
In Mexico, the healthcare system urgently needs to be redesigned, as more than 50 million Mexicans lack access to healthcare, while public spending on this area is only 6.2% of the gross domestic product (GDP), well below the 8.8% average for member countries of the Organization for Economic Cooperation and Development (OECD).
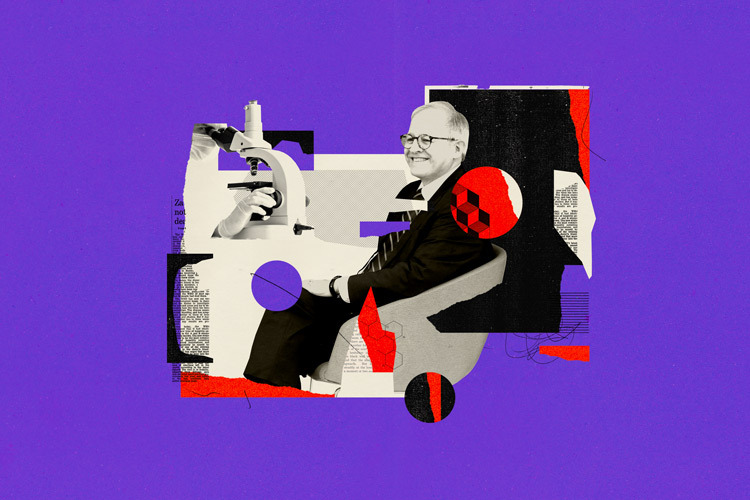
“How do we design a system for everybody is an open question,” said Peter Jones, research professor at the School of Architecture, Art and Design (EAAD) and Faculty of Excellence at Tec de Monterrey, during his presentation “Designing the Health System for the Future of Mexico” at the Horizontes en Salud forum, organized by Tec de Monterrey, The Next Decade and Distrito Tlalpan.
In his native Canada, Jones has worked in service and systems design, applying the design thinking methodology, which focuses on understanding user needs through empathy and finding innovative and feasible solutions to their problems.
This methodology almost always begins with the question, “How may we…?” , encouraging teamwork, flexibility, and creativity.
Since arriving at Tec —following a successful career at OCAD University in Toronto, Canada— Jones has moved away from traditional infrastructure-focused approaches, leaning into one that combines systems thinking, participatory design, and future-thinking to transform or create complex healthcare services.
“It’s not just about implementing technology, but about how systems are built and how to best address the root causes of the problem,” Jones said.
A look at the Structural Challenges
During his presentation, the researcher identified some critical factors that the Mexican health system will have to face in the coming years, such as a rapidly aging population, disparities in healthcare access between rural and urban areas, poverty and inequality, an increase in chronic diseases, the mental health of young people, migration and gender inequalities.
“We must address the core issues, because the impacts will become problems that are beyond the ability of design, engineering, basic science, and healthcare to address,” the expert said.
For Jones, the biggest challenge is to redesign the system from the root causes, with an emphasis on prevention.
Over the years, the researcher has worked on the application of systemic design—an approach that considers the complexity and interconnections of a system, seeking sustainable and innovative solutions—at different levels.
One example is the Sea Change project, which works with primary care physicians to implement clinical guidelines for cardiovascular disease. The goal is to integrate prevention and self-care into daily practice. He emphasized that this type of innovation doesn’t require complex technologies, but rather a system redesign that empowers people to monitor their symptoms themselves.
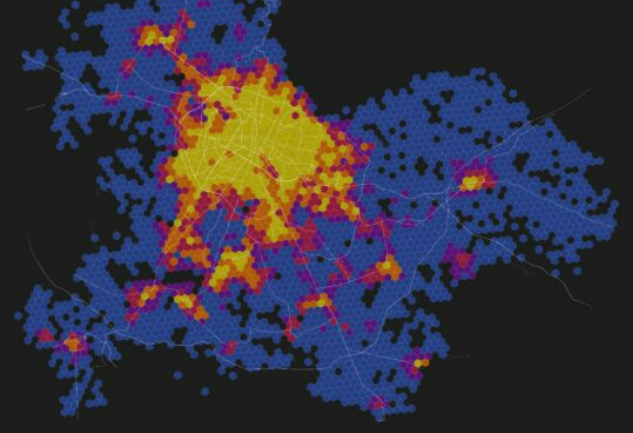
One of the key strategies for applying this way of thinking to systems design is visualizing futures through the three-horizon model, which allows us to observe how current solutions lose effectiveness, what new practices emerge, and how to imagine a third horizon where health systems respond appropriately to the needs of their populations.
“What the downward curve of the current era shows is the decline of the solutions and the processes of today that are losing effectiveness, the middle curve is the innovations that are taking shape and will lead to the future third horizon,” he explained.
Collaborative Tools, Shared Knowledge
While systemic design is not a quick way to redesign and rethink an entire system, it is a robust and long-lasting way of doing so, promising the satisfaction and well-being of the entire population.
During the talk, he explained the seven-stage methodology, which combines systems thinking with design thinking: framing the system, listening to the system, understanding the system, visualizing the desired future, exploring the possibility space, planning the change process, and driving the transition.
In his view, one of the greatest areas of opportunity to improve Mexico’s healthcare system is social prescription, a model in which doctors not only prescribe medications but also lifestyle changes, emotional support, and access to healthy food and decent housing. He also emphasized the importance of strengthening prevention through primary care, facilitating self-care and early diagnosis of chronic diseases.
He then spoke about the need to develop accessible and personalized digital platforms in Spanish that allow patients and professionals to manage health information clearly and effectively.
Later, he mentioned the value of creating new models of decentralized care, with available services that are beyond traditional hospitals, including in pharmacies or mobile clinics. “That’s already being done here ,” Jones said.
Another line of action is leveraging telemedicine as an integral part of the system and transforming hospitals into open spaces integrated with the community, offering a variety of health and prevention services. “They already look like they’re halfway there, but are not there yet”, the researcher emphasized.
Finally, he highlighted that innovation in health care does not have to depend exclusively on the government or large investments; there is room for social entrepreneurship, interdisciplinary collaboration, and the creation of community support networks that strengthen the social fabric and contribute to more equitable, efficient, and humane care.
“All of these challenges have entrepreneurial and research applications, and they all require us to work together,” Jones said.
Were you interested in this story? Want to publish it? Contact our content editor to learn more: marianaleonm@tec.mx