You’ve likely heard about menopause in family conversations or on social media. But what exactly is it? Why does it cause symptoms in 80% of women who reach this stage? And how does it impact their quality of life? Experts break it down and share therapies and treatments that might offer viable solutions.
Menopause is the point in a woman’s life that generally begins after she has gone 12 months without a menstrual period. This occurs because the ovaries stop producing hormones, particularly estrogens responsible for various bodily functions.
Typically, menopause occurs naturally between the ages of 45 and 55, though it can happen earlier in women who have had surgeries to remove their ovaries or uterus or those who have undergone specific cancer treatments.
What Are the Symptoms of Menopause, and Why Do They Occur?
Before menopause, there is a transitional stage where the ovaries gradually produce less estrogen, known as pre-menopause or perimenopause. During both this period and the years following menopause, a wide range of symptoms can appear, significantly impacting women’s lives.
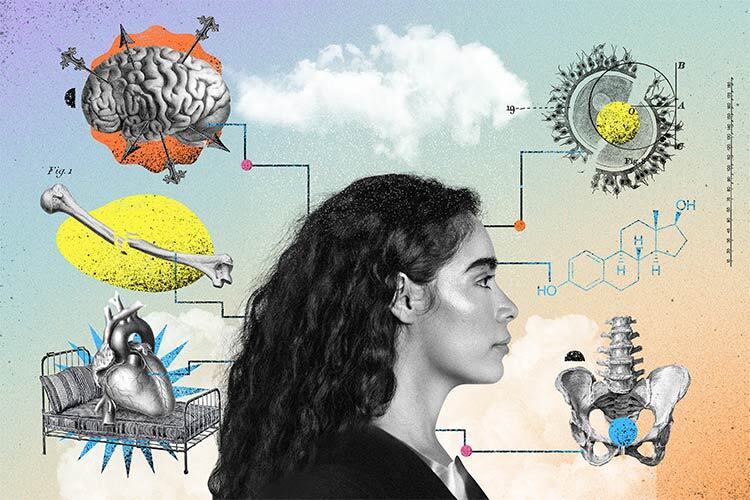
These symptoms are due to the lack of estrogen, a group of hormones playing a crucial role during the menstrual cycle by stimulating ovulation and preparing the uterus to receive an embryo in case of fertilization. Additionally, estrogens have many other functions related to bone health, heart and blood vessel function, cognitive functions, as well as skin and hair lubrication.
Therefore, the decrease or loss of estrogen production during pre and postmenopause “affects all body systems,” explains Dr. Carlos Félix Arce, a gynecologist specializing in menopause at TecSalud, in an interview with TecScience.
“The most common symptom of menopause is the infamous hot flashes,” a sudden sensation of heat that starts in the chest and spreads throughout the body. Approximately 80% of women experience this, along with palpitations and sweating, collectively known as “vasomotor syndrome.”
However, Dr. Arce notes that there are many more manifestations caused by hormone deficiency: “There are about 20 symptoms, and many of them are not easily recognized by the affected person.”
These include psychological and psychiatric symptoms such as sadness, depression, anxiety, distress, irritability, easy crying, and panic attacks. Women may also experience joint pain, arthritis, dry skin and vaginal dryness, lack of energy, loss of sexual desire, involuntary urine leakage, and cognitive issues related to concentration and memory loss.
The most severe symptoms, which can be life-threatening, include cardiovascular diseases —the leading cause of death among women nationwide— and osteoporosis. “Around 28% of women experience decreased bone calcium, and 2.8% suffer from severe osteoporosis,” the expert notes.
Despite the dangers posed by cardiovascular conditions and osteoporosis, Dr. Arce stresses that hot flashes, as well as psychological and cognitive symptoms, should not be underestimated: “Imagine not sleeping for a night due to a hot flash or sweating episode; how would you feel the next day?”
All these symptoms can severely impact the quality of life of women, who, in some cases, as Dr. Arce explains, “are so affected that they can’t function normally. They describe themselves as ‘dead alive,’ unable to live their lives normally.”
What Treatments Can Improve Menopausal Symptoms?
Currently, the most effective treatment for menopausal symptoms is hormone replacement therapy (HRT), which involves taking hormones, especially estradiol, a type of estrogen. This therapy is supported by the largest study to date, conducted by the Women’s Health Initiative (WHI), which reviewed data from over 160,000 postmenopausal women over several decades.
In 2002, a preliminary analysis of this data suggested that HRT could increase the risk of breast cancer, cardiovascular disease, and pulmonary and cerebral embolism. However, after collecting more data over another 20 years, the same research group realized that their initial conclusions were biased due to the inclusion of many older women.
Reanalyzing the records, they concluded that the benefits of HRT outweigh the risks for women under 60 without a history of breast cancer.
Their 2023 results highlight that HRT does not increase mortality or cardiovascular disease risk and reduces bone fracture risk by 33% while almost entirely alleviating vasomotor syndrome symptoms. Other studies have found that HRT also relieves anxiety and vaginal dryness.
Preventive measures also include lifestyle changes. “Negative habits like smoking, drinking alcohol, and not exercising should be abandoned. It’s about a comprehensive management of women in this stage,” Dr. Arce emphasizes.
Despite HRT potentially being a viable and effective option for many women, there is still a lot of misinformation and lack of knowledge on the subject, both among the general public and medical professionals.
“Some doctors, upon learning that a patient is on HRT, advise against it, claiming it’s too risky. The idea that hormones should not be taken is deeply ingrained,” says Dr. Arce, who concludes: “Yes, there is a risk factor, but the vast majority of women do not experience any problems.”
According to the 2023 WHI research, HRT slightly increases the risk of breast cancer. Among a population of women aged 50 to 59 who take HRT for five years, the increased risk is equivalent to three new cases of breast cancer per thousand women, which is similar to the increased risk of developing this cancer from consuming one to two alcoholic drinks per day.
Are you interested in this story? Would you like to publish it? Contact our content editor for more information: marianaleonm@tec.mx.