For decades, obesity has been primarily defined through the Body Mass Index (BMI), a measure that relates weight to height. However, recent analyses have shown that this tool is insufficient for accurately diagnosing obesity as a disease, given that it is a highly complex condition influenced by genetic, metabolic, and environmental factors.
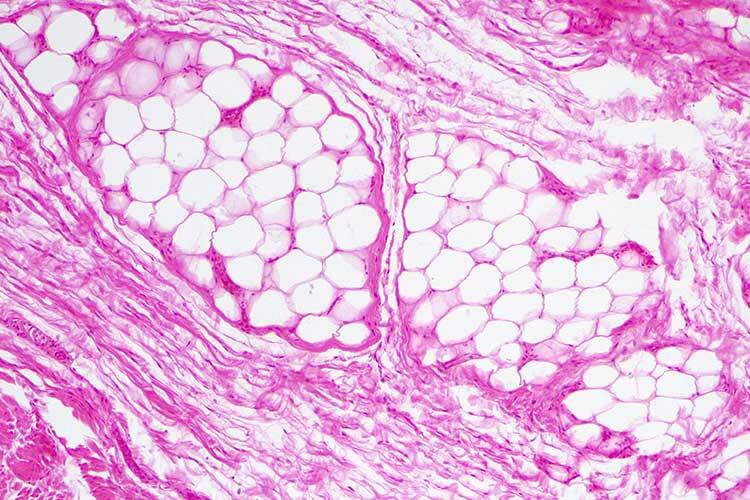
Obesity is a condition characterized by excessive adiposity (a measure that calculates body fat), with or without abnormal distribution or function of adipose tissue, and has multifactorial causes, according to a definition developed by a team of more than 50 doctors and scientists in the latest report published on January 14, 2025, in the British medical journal The Lancet Diabetes and Endocrinology.
“It is important to understand that not all individuals with obesity are sick. There are two main groups of patients: those who are metabolically healthy and those who are metabolically unhealthy,” said David Kershenobich, physician and researcher from the Faculty of Medicine at the National Autonomous University of Mexico (UNAM) and currently Mexico’s Secretary of Health, in a previous statement to TecScience.
The Difference Between Clinical and Preclinical Obesity
In most cases, obesity is a multifactorial disease caused by an obesogenic environment, psychosocial factors, and genetic variants. According to the World Health Organization (WHO), an obesogenic environment exacerbates the likelihood of obesity in individuals and populations due to structural factors that limit access to healthy food, social barriers to physical activity, and the lack of appropriate regulatory measures.
However, clinical obesity is defined in The Lancet report as a chronic, systemic disease characterized by alterations in the function of tissues, organs, the entire organism, or a combination of these, due to excess adiposity.
Clinical obesity can cause severe damage to vital organs, leading to life-altering complications and even life-threatening conditions (e.g., heart attack, stroke, and kidney failure).
On the other hand, preclinical obesity refers to a state of excess adiposity with preserved function of other tissues and organs. It carries a variable but generally high risk of progressing to clinical obesity and other non-communicable diseases (e.g., type 2 diabetes, cardiovascular diseases, certain types of cancer, and mental health disorders).
Although the risk of mortality and obesity-related diseases may progressively increase with fat accumulation, distinguishing between preclinical and clinical obesity (i.e., healthy vs. disease) serves both clinical and policy-making purposes.
Next Steps for Clinical Diagnosis
Individuals with confirmed obesity (i.e., excess adiposity with or without abnormal function of organs or tissues) should be evaluated to determine whether they have clinical obesity.
The diagnosis of clinical obesity requires one or both of the following main criteria, as outlined in The Lancet: evidence of reduced organ or tissue function due to obesity (i.e., signs, symptoms, or diagnostic tests indicating abnormalities in one or more tissue or organ systems); or substantial age-adjusted limitations in daily activities that reflect the specific impact of obesity on mobility or other basic functions of daily life (e.g., bathing, dressing, using the toilet, maintaining continence, and eating).
What Is the Body Mass Index?
The Body Mass Index was first proposed by Belgian mathematician Lambert Adolphe Quetelet in 1832. It is calculated by dividing a person’s weight by the square of their height and has long been used to determine whether a person is obese.
Previously, BMI alone was used to assess whether an individual had obesity. However, the updated report now focuses on how excess body fat—adiposity—affects the body.
In recent years, researchers have demonstrated that BMI is inadequate for diagnosing clinical obesity.
For example, in individuals of European descent, obesity is typically defined as having a BMI of 30 or higher, which is associated with a high level of body fat. However, an athlete with significant muscle mass could be classified as obese based on BMI, while someone with a “normal” BMI could have excess fat that increases their risk of serious health issues, explained Francesco Rubino, a bariatric surgeon at King’s College London, in Nature following the new definition proposed by the team he led.
Nonetheless, as a valuable tool, the 2025 report authors propose using BMI only as an indirect measure of health risk at the population level, in epidemiological studies, or for screening purposes—not as an individual health indicator.
Excess adiposity should be confirmed through direct body fat measurement when available or by at least one anthropometric criterion (e.g., waist circumference, waist-to-hip ratio, or waist-to-height ratio), in addition to BMI, using validated methods and appropriate cut-off points based on age, gender, and ethnicity.
In individuals with a very high BMI (i.e., >40 kg/m²), however, excess adiposity can be pragmatically assumed without requiring additional confirmation.
What If I Am Diagnosed with Clinical or Preclinical Obesity?
In Mexico, 36.9% of adults live with this condition, and by 2030, this figure could reach 45%, according to the National Institute of Public Health (INSP) in a 2024 report. Additionally, 36.5% of school-aged children and 40.4% of adolescents are overweight or obese, according to UNICEF.
People with clinical obesity should receive timely, evidence-based treatment aimed at improving (or remitting, when possible) obesity-related clinical manifestations and preventing further damage to vital organs.
Those with preclinical obesity should receive evidence-based health counseling, ongoing monitoring of their health status, and, when applicable, appropriate interventions to reduce their risk of developing clinical obesity and other related diseases, depending on their individual risk level.
Despite estimates that half of the population has this condition, only 1% receive proper treatment designed specifically for each patient—rather than solely addressing symptoms and comorbidities—said Carolina Solis-Herrera, Chief of the Division of Endocrinology at the University of Texas, in 2024.
Myths and Stigmas About Obesity
It’s not just about having a high weight: Overweight is simply a condition characterized by excessive fat accumulation. However, it does not automatically meet the criteria for a chronic disease diagnosis. Still, it is associated with an increased risk of various conditions such as type 2 diabetes and heart disease.
It’s not just about going for a run to lose weight: Clinical obesity is a public health issue. Policymakers and health authorities must ensure adequate and equitable access to evidence-based treatments for people with clinical obesity, just as they would for any other chronic and potentially life-threatening disease. This counters the widespread misconception that obesity should be addressed solely through individual solutions.
It’s not just about eating salads and light meals: While many assume obesity is solely linked to diet, it is actually a multifactorial problem involving genetic predispositions, mental health conditions, socioeconomic factors, limited access to healthy food, an obesogenic environment, and public policies, according to Marco Rito, director of the IOR at the International Congress on Obesity Research.
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx