In 2010, Doug Olson, an American man based in California, became one of the first people to be cured of cancer with a novel immunotherapy called CAR-T cells.
Olson had battled for years with chronic lymphocytic lymphoma —a type of blood cancer that affects B lymphocytes, the white blood cells that create antibodies— that didn’t respond to existing treatments.
After receiving said therapy, his cancer disappeared, and he remained in remission for over a decade. Today, he’s still alive and active. He even runs marathons.

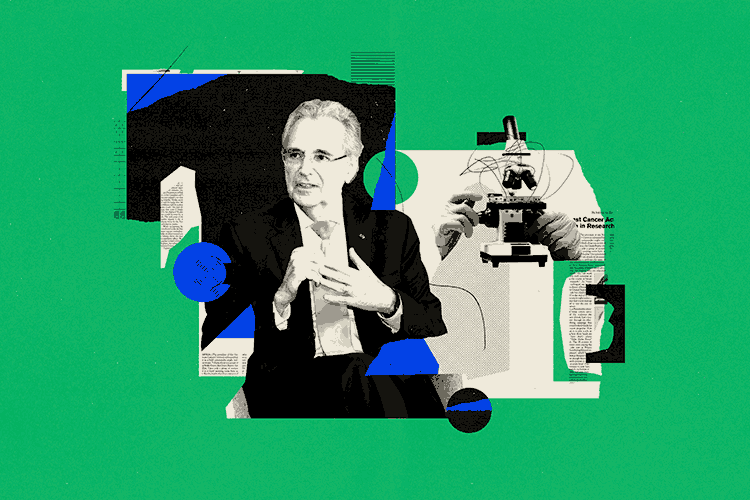
His case marked the beginning of a new era in the battle against cancer. “He was about to die, and they gave him this thing, and he was cured,” says José Carlos Crispín-Acuña, a research professor at the School of Medicine and Health Sciences (EMCS) at Tec de Monterrey and the Salvador Zubirán National Institute of Medical Sciences and Nutrition (INCMNSZ). “It became a therapy that many people began to believe in.”
In CAR-T cell therapy, T cells —a type of white blood cell that detects and destroys abnormal or invading cells— are extracted from the sick patient.
In the laboratory, these cells are modified to express a receptor, called CAR, which recognizes an antigen present on the cells to be attacked —tumor cells in the case of cancer.
These modified cells then multiply and are reinfused into the patient. Once inside, they can recognize and destroy malignant cells.
However, in countries where it’s available, such as the United States and some in Europe, it can cost up to a million dollars. Fortunately, ·there are those of us who are developing these therapies on a non-profit basis, intending to make them available to people,” says Crispín-Acuña.
Advanced Therapies for the Future of Medicine
CAR-T cells are part of advanced therapies, a group of innovative medical treatments that utilize cells, genes, or tissues to repair, replace, regenerate, or improve bodily functions.
These include gene therapies, which utilize genes to treat diseases; cell therapies, which employ modified or selected cells, such as CAR-T cells; and tissue engineering, where tissues, including skin, are created or modified to repair or replace them.
These have begun to transform the care of the most difficult-to-treat conditions, such as autoimmune, rare, or degenerative diseases, and cancer.
“These are relatively new therapies that have a lot of potential,” says Crispín-Acuña. Given their promise, he and an interinstitutional group of scientists began creating a network focused on developing them in Mexico.
On June 12 and 13, 2025, TecSalud, the EMCS, the INCMNSZ and the National Academy of Medicine, organized a symposium entitled Advanced Therapies: Innovation for Major Health Challenges, bringing together researchers from these institutions, as well as from the National Polytechnic Institute (IPN), the National Autonomous University of Mexico (UNAM), the National Institute of Genomic Medicine (INMEGEN), the University of Navarra, the University of Salamanca and others.
The presence of Spanish researchers was crucial, as they are leading the way in this type of treatment aimed at a broad population, with the Spanish Network of Advanced Therapies (TERAV).
“They’re a group of dedicated individuals who’ve applied for funding together and helped each other with the regulatory processes,” says Crispín-Acuña. “They’re our role model.”
The Future of CAR-T Cells in Mexico
In his laboratory, Crispín-Acuña, together with Alejandro Madrigal, a hematologist and researcher at EMCS and the Faculty of Excellence at Tec de Monterrey, and numerous researchers and students, is developing new applications for CAR-T cells through in vitro studies in cell lines and animal models.
Specifically, they are focusing on finding ways to use CAR-T cells to treat myeloid leukemia —a type of cancer related to the bone marrow— and brain cancer.
“So far, no one has been able to develop a CAR-T against these,” Crispín-Acuña says.
To date, CAR-T cells have shown the greatest success in so-called “liquid” cancers, i.e., those affecting the blood, bone marrow, and lymphatic system. Now, thanks to new advances, they are beginning to be used in solid tumors —such as lung cancer— and autoimmune diseases.
The benefits of these are that they are highly effective in treating difficult diseases, they are manufactured from the patient’s own cells—reducing the risk of immune rejection—and a single infusion can be sufficient for a cure.
However, there are also risks, such as toxicity, as well as overactivation or inactivation of the immune system.
“One of the first patients given CAR-T cells was cured of cancer, but died of COVID-19,” Crispín-Acuña warns. “We mustn’t forget that these are therapies for deadly diseases.”
In the future, Crispín-Acuña, along with researchers in Mexico and around the world, seeks to develop CAR-T cells that can exclusively attack cancer cells without destroying healthy tissue.
Although the development of these and other advanced therapies in Mexico is still in its early stages, they hold promise for treating diseases we never thought possible.
“A few years ago, the idea that the immune system can attack cancer was revived,” says Crispín-Acuña.
Were you interested in this story? Want to publish it? Contact our content editor to learn more: marianaleonm@tec.mx