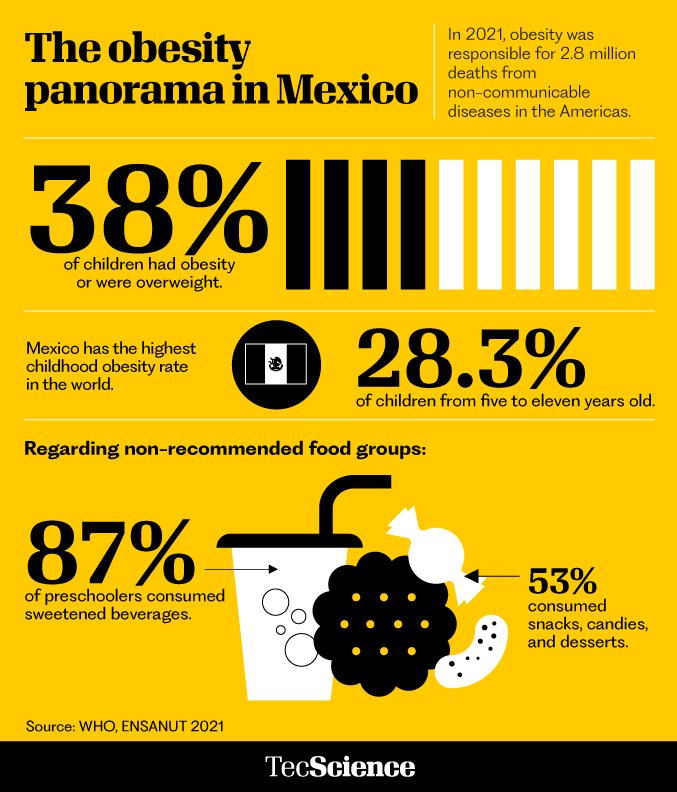
The problem is a large one, affecting us since childhood. According to the United Nations Children’s Fund (UNICEF), one in three Mexicans under the age of 19 was overweight in 2021.
Over the past decade, the onset of obesity has occurred at increasingly earlier ages, thus impacting key development stages.
Paradoxically, some of the tools that science proposes to solve the problem are small but powerful ones. How small are they? 800 times smaller than a human hair or the size of a drop of blood.
Nanoparticles measure a billionth of a meter and using them is one of the innovations proposed by specialists at Tec de Monterrey’s Institute for Obesity Research (IOR), created in 2022.
These experts are also constructing diagnostic tests that use a few drops of blood to detect metabolic diseases before they present symptoms, examine how breast milk is involved in these diseases, and propose public policies based on these investigations.
Nanoparticles, a fantastic voyage
For decades, the term “nanotechnology” was a novelty. Years before the movie Fantastic Voyage came out in 1966, in which a team of scientists is miniaturized to enter the body of a wounded man and save his life, physicist Richard Feynman had already suggested the possibility of manipulating matter at a nanometric scale, using molecules as the building blocks for creating robots that could be injected into the bloodstream.
Today, nanotechnology is being used to deliver drugs to specific tissues. That’s what researcher Omar Lozano is working on.
The engineering physics specialist is part of IOR’s Bioengineering and Medical Devices unit, a multidisciplinary team of physicists, biologists, immunologists, biotechnologists, and doctors who are designing nanoparticles to combat obesity.
For this to be viable, nanoparticle materials have to be biocompatible and not interfere with the functions of pharmaceuticals. They tend to use natural polysaccharides, noble metals (that don’t have chemical reactivity), and biodegradable polymers, which are those used at the IOR because they are low cost and could be mass produced in the future.
There are different techniques for creating these particles, such as emulsification, ionic gelation, and nanoprecipitation. At the IOR, they use nanoprecipitation: through sound waves, they create drops that encapsulate drugs in nanoparticles measuring less than 150 nanometers.
In Fantastic Voyage, the submarine navigates through the arterial system to arrive at the brain. But you don’t need to control nanoparticles. They know where to aim for through a kind of magnet on their surface.
These magnets can be a peptide, a sequence of amino acids, a protein, or an antibody that attracts them toward the target cell.
This treatment is designed above all for children because people who were obese in their childhood or adolescence are five times more likely to be obese as adults. However, at least seven years will elapse before clinical trials can begin.

Infographics: Oldemar González / TecScience
Detecting obesity in a few drops of blood
The most common way to detect obesity is the Body Mass Index (BMI), which relates people’s height to their weight. However, this method cannot detect metabolic diseases or provide early detection of those who will become obese.
That’s why Mirna González from the IOR’s Bioengineering and Medical Devices unit proposes creating tools to detect metabolic disorders from childhood, identifying the proteins present in the blood that indicate preobesity.
The quantities have to be measurable in small amounts, as they intend to do so with small devices, which act like a rapid test: one small sample (a few drops of blood) flows through the device and it gives a diagnosis when it identifies the molecules of interest.
González hopes to have prototypes in under two years and plans to integrate three protein searches into one single device. At the moment, Ph.D. student Margarita Ortiz is developing the tests at the University of Houston.
Once they’re ready, they’ll compare their performance with that of conventional tests, first in adults and then in Mexican children.
Since 2011, Mexico’s obesity figures have increased. (Illustration: Arturo M. Reyes / TecScience)
From the mother’s breast
Cuauhtémoc Licona from the IOR’s Integrative Biology unit is studying microbial systems and analyzing breast milk, as we know that the composition of each microbiota is an indicator of people’s health.
Our microbiota is a community of organisms that inhabit our skin, mouth, vagina, or intestines and protects us from infections. The mammary gland has one of its own.
Each milliliter of breast milk contains a million bacteria. This food imparts good microorganisms to a newborn’s intestines. We know that, during childhood, the variety and abundance of gut microbiota are lower if the BMI is higher.
Licona is the director of the FEMSA Biotechnology Center and led the first Mexican study to compare the microbiota in people’s colostrum with gestational diabetes and obesity, people with obesity, and people without obesity.
After analyzing 43 samples of colostrum, they observed that gestational diabetes and obesity leave a mark.
Obesity favors the group of firmicutes, particularly staphylococci, which are bacteria linked to metabolic diseases.
To complete what Licona calls “the snapshot,” he and Marion E. G. Brunck, from the IOR’s Experimental Medicine and Advanced Therapies unit and coauthor of the study, analyzed leukocytes from the colostrum (related to the immune system), detecting fewer B lymphocytes (a type of leukocyte) in the presence of obesity.
The aim of this research is to create treatments with probiotics, living organisms that are beneficial to people’s health.

Brunck emphasizes that this information is not intended to stigmatize or criticize mothers living with obesity. Rather, the idea is to find answers about how much their immune status is manifested in breast milk and how this impacts the baby. (Photo: Udell Jiménez / TecScience)
Including science in public policy
Researchers from the IOR’s Public Policy unit, together with Daniel Bernal, doctor and coordinator of the public policy and health initiative at the School of Government and Public Transformation, conducted a study on the effect of public policies on children under the age of five, such as diet guidelines, RDI labeling, and taxes on sweetened beverages and products with a high calorie density.
They found that despite a downward trend in children’s BMI from 2005 to 2010, there was a constant increase in childhood obesity from 2011, one year after the National Agreement for Healthy Nutrition (which sought to generate changes in schools).
Bernal believes this is because policies have not been able to achieve synergy in tackling the factors of obesity, which is why he says that policies must be designed with scientific evidence to support what modifies behavior and to what extent.
He warns that, as childhood and adolescent obesity have multiplied by a factor of 10 over the past 40 years, it is imperative to prevent it, identify it in time, and have different treatments available.
As Omar Lozano says: “This is a very extensive topic. Saying that we’re going to solve it with a small team is very arrogant. In reality, it’s going to take a lot of work.”
Infographics: Oldemar González / TecScience