Fortino Salazar, a neurologist, surgeon, and researcher at the Tecnológico de Monterrey, is part of a group of experts in neurosciences at the Center for Parkinson’s, Movement Disorders and Neurorestoration at the Zambrano Hellion Hospital of the TecSalud system.
Since 2015, the group has focused on doing cutting-edge research and providing comprehensive and multidisciplinary treatment to people who suffer from it.
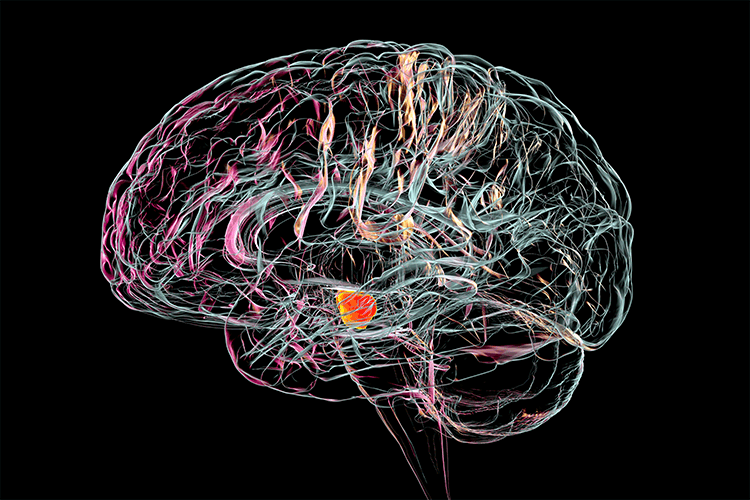
Héctor Ramón Martínez, director of TecSalud’s Institute of Neurology and Neurosurgery, defines the disease as the loss of the substantia nigra in which important symptoms, such as coordination problems, tremor, stiffness, and slow movement are present.
Parkinson’s is a degenerative neurological disease that affects the brain and those parts of the body controlled by it, resulting in problems with movement. It is caused by the low production of dopamine −an important neurotransmitter− and affects more than 8 million people worldwide.
New Parkinson’s treatment
Parkinson’s disease is an area of continuous research where it is sought to obtain better and better treatments, or to optimize those that already exist, to give people who live with it the opportunity to live a fulfilling life.
One thing that is being worked on is genetic studies to detect gene variants that predispose people to this condition.
In collaboration with the University of Cleveland, Daniel Martínez Ramírez, research neurologist, and other experts from Tec de Monterrey, are seeking to identify Latin American genes from Parkinson’s patients, to see if there are region-specific traits that can be worked on to improve treatments.
For Salazar and Martínez Rodríguez, the future of treatments against Parkinson’s is promising, but currently, doctors already have great tools. “Nowadays, there are many treatment alternatives to help them cope with the disease in the best way possible”, says Salazar.
“You can have a happy, complete, and satisfying life with Parkinson’s disease”, concludes Martínez Rodríguez.
Deep brain stimulation, an innovative therapy
Once someone has been diagnosed with Parkinson’s, there are different ways to deal with the disease. When it isn’t very advanced, drugs that increase the production of dopamine in the brain are usually administered.
When medications and motor rehabilitation therapies are no longer enough, there is an innovative procedure called deep brain stimulation, in which Salazar specializes.
“Before doing the operation, we do a very strict evaluation to find out if the patient could benefit from it,” says Salazar. The procedure consists of placing electrodes deep in the brain that are connected to a device that sends small electrical pulses.
The device, similar to a pacemaker, is placed under the skin of the chest. A wire connects the electrodes placed on the brain and the device. The pulses stimulate the areas of the brain that control movement and other aspects related to the symptoms that each person presents, reducing the symptoms.
In the long term, this technique gives patients a better quality of life for a long time. “We have patients who had the surgery almost 10 years ago and still benefit from it,” he says.
In addition, at the Center for Parkinson’s, Movement Disorders, and Neurorestoration, patients are cared for by a variety of specialists who see each of their symptoms, depending on which ones they have.
“The plan is to have a complete and comprehensive treatment, not just medication or surgery,” says Salazar. Specialists in rehabilitation, nutrition, urology, gastroenterology, neuropsychology, and cardiology, among others, converge at the center.
Parkinson’s disease symptoms: More than shaking
In general, when we think of this condition, we imagine a person whose hands are shaking, however, it is much more than that. “There is a very broad group of symptoms known as non-motor symptoms,” explains Salazar.
Some of the most common are difficulties with smelling or swallowing, chronic constipation, urinary problems, sleep disturbances, memory problems, depression, and other neuropsychiatric conditions.
Until recently, even when diagnosing, the approach related to mobility problems predominated. According to this, Parkinson’s is classified into two types: when the patient’s limbs tremble at rest or when they have slow movements and stiffness in the limbs.
Under this idea, many experts had observed that those with a profile where they trembled had a slower progression of the disease, while those with a rigid profile showed a more rapid and severe evolution.
“This is how teachers taught me, they told me that those who tremble seem to do better,” recalls Daniel Martínez Ramírez, a research neurologist at Tec de Monterrey with more than 10 years of experience in treating patients with Parkinson’s.
However, according to Martínez Ramírez, there is increasing evidence that this is not necessarily the case and that the profiles can become mixed over time. Today, surgeons and specialists are increasingly focusing on non-motor symptoms.
In a study for his doctoral thesis, the researcher found that patients who have a profile where symptoms related to the autonomic nervous system predominate, such as gastrointestinal or urinary issues, have a higher risk of hospitalization and even death.
That is why, in his practice, it has become very relevant to observe and monitor all the symptoms, so he can achieve early detection of the type of symptoms that predominate and in turn be able to provide individualized treatment that improves the quality of life of patients in the long term.