About one in 10 breast cancer cases are linked to inherited genetic mutations. As a result, international clinical guidelines recommend risk assessments for individuals with a family history of breast, ovarian, or gastrointestinal cancers.
Genetic counseling plays a key role in the prevention and management of hereditary breast cancer. After undergoing genetic testing, individuals at risk can be identified, informed, and provided with recommendations for monitoring studies, preventive surgeries, or specific medications to reduce their risk.
However, access to these programs is limited in countries like Mexico. TecSalud Breast Cancer Center and the National Institute of Clinical Sciences and Nutrition Salvador Zubirán have implemented genetic risk assessment services, providing care to patients referred from other centers.
Researchers from both institutions later evaluated the impact of genetic counseling and the barriers that hinder patients from adopting recommended preventive measures. The study was published in JCO Global Oncology.
Study on the Impact of Genetic Counseling
The study involved women and men with mutations associated with an increased risk of breast cancer (including BRCA1, BRCA2, CHEK2, PALB2, ATM, NF1, RAD51C, PTEN, and TP53 genes), who had received a medical explanation of their genetic test results at least six months prior.
Participants were invited to respond to a survey exploring whether they had undergone monitoring studies or preventive surgeries, as well as the challenges they faced. The study also analyzed whether genetic testing had been conducted on relatives at risk of having a mutation.
Most participants were women (88%), had public health coverage (53%), and were diagnosed with breast or ovarian cancer (61%). Overall, 87% were aware that they had a genetic mutation, and 80% knew that this mutation increased their risk of developing new cancers.
Adoption of Preventive Measures
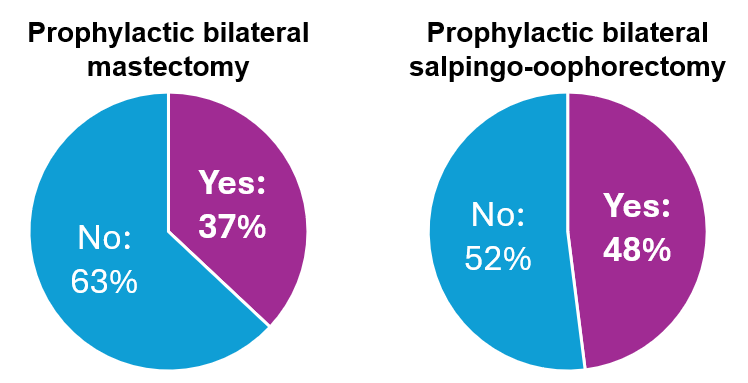
Depending on the type of mutation, 37% of candidates underwent preventive bilateral mastectomy, and 48% had preventive surgery on their fallopian tubes and ovaries.
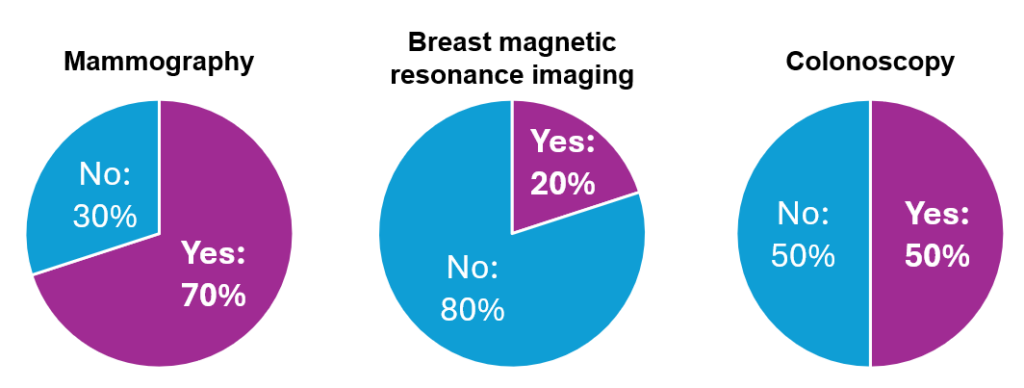
Regarding monitoring studies, 70% of participants had an annual mammogram in the past year, and 20% had a breast MRI in the previous year—additionally, 50% of those who were recommended to have a colonoscopy followed through with the procedure.
The main barriers that hindered participants from taking measures to reduce their cancer risk were financial limitations (67%), the perception that their doctor had not recommended the studies or surgeries (35%), and fear (24%).
On the other hand, attending follow-up oncology consultations was associated with a higher likelihood of undergoing monitoring studies and preventive surgeries.
In total, 87% of individuals with a genetic mutation also encouraged their relatives to undergo genetic risk assessment.
Sixty-three percent of families underwent genetic testing. Having a close relative recently diagnosed with cancer and considering the genetic evaluation program useful increased the likelihood of initiating testing within families with a mutation.
Implications of Genetic Counseling
Despite the barriers patients face, this study observed considerable adoption rates of cancer risk reduction measures and genetic testing in families.
Therefore, it is crucial to implement targeted strategies to reduce out-of-pocket expenses for patients, improve communication between patients and doctors, encourage attendance at follow-up consultations, and promote a clear understanding of what it means to have a mutation.
These steps will increase the benefits of genetic counseling, allowing individuals with mutations and their families to take proactive measures to safeguard their health.
Hereditary Breast Cancer Risk Criteria
- You or a family member was diagnosed with breast cancer before age 50.
- Your mother, sister, or daughter has had breast or ovarian cancer.
- Two or more people in your family have had breast and/or ovarian cancer.
- You or a family member has had cancer in both breasts.
- A man in your family has had breast cancer.
- Two or more people in your family have had breast and/or gastrointestinal cancer.
.
Editor’s Note: If you meet any of these hereditary breast cancer risk criteria, visit healthcare services to inquire about genetic testing and counseling.
References
1. Buys, S. S. et al. A study of over 35,000 women with breast cancer tested with a 25-gene panel of hereditary cancer genes. Cancer 123(10), 1721-1730 (2017).
2. Daly, M. B., Pilarski, R., Berry, M. P. & Buys, S. S. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic. NCCN Clinical Practice Guidelines in Oncology (2019).
3. Ashton-Prolla, P. et al. Development and validation of a simple questionnaire for the identification of hereditary breast cancer in primary care. BMC Cancer 9(1), 283 (2009).
4. Aguilar y Méndez, D. et al. Enhancing access to genetic cancer risk assessment (GCRA) in Monterrey, Mexico: The beginning of a prevention program. Journal of Clinical Oncology 37(15), e13150 (2019).
5. Strasser-Weippl, K. et al. Progress and remaining challenges for cancer control in Latin America and the Caribbean. The Lancet Oncology 16(14), 1405-1438 (2015).
6. Chavarri-Guerra, Y. et al. Abstract P6-09-05: Factors associated with the uptake of risk-reducing surgeries among Hispanic women at high risk of breast and ovarian cancer. Cancer Research 78(4), P6-09-05 (2018).
7. Blazer, K. R. et al. Development and Pilot Implementation of the Genomic Risk Assessment for Cancer Implementation and Sustainment (GRACIAS) Intervention in Mexico. JCO Global Oncology 7(1), 992-1002 (2021).
.
Authors
Fernanda Mesa Chávez. She holds a degree in Medicine and a Master’s in Biomedical Sciences from Tecnológico de Monterrey. She currently serves as the Coordinator of the Oncology Research Group at TecSalud’s Breast Cancer Center. She has published 18 articles in internationally indexed journals and 30 abstracts at international conferences. Her scientific interests focus on breast cancer research and the design and implementation of research projects with direct clinical applications to improve patient care and well-being.
Mauricio Zegarra López. A newly graduated physician from the 40th class of the School of Medicine and Health Sciences at Tecnológico de Monterrey. He is completing his medical internship in the Oncology Research Group at TecSalud’s Breast Cancer Center. In addition to his studies, he assists as a teaching assistant in clinical case studies during the Gynecology and Obstetrics rotation.
Cynthia Villarreal Garza. Director of the Oncology Institute at TecSalud. She founded and directs “Joven & Fuerte: Program for the Care and Research of Young Women with Breast Cancer.” Co-founder of the civil association “Doctors and Researchers in the Fight Against Breast Cancer.” Since 2007, she has been a professor at Tecnológico de Monterrey. Cynthia has published over 150 indexed articles and is a Level II member of Mexico’s National System of Researchers. Her projects are primarily dedicated to improving the lives of breast cancer patients in Mexico.
.