For the first time in history, a multidisciplinary team of scientists managed to reverse type 1 diabetes in a 25-year-old patient, who received a reprogrammed stem cell transplant and less than three months later she started producing her own insulin.
She is the first human with type 1 diabetes to be treated using cells that were extracted from her own body. The results of his case were published on the specialized site Cell and the success of the procedure is already considered a milestone for modern medicine.
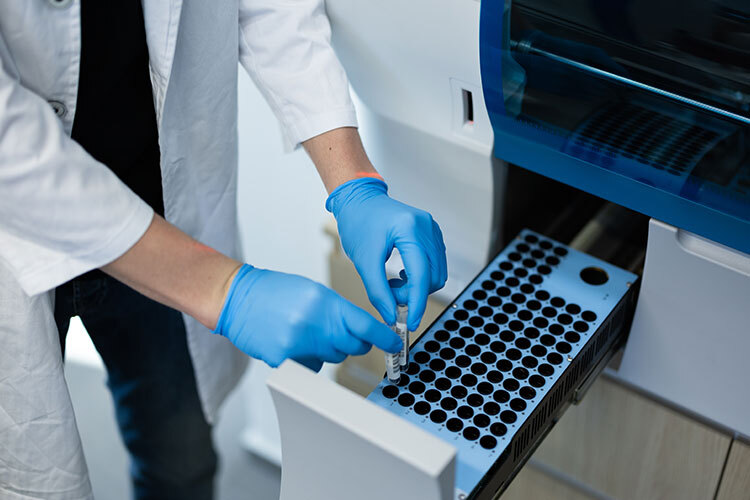
The paper, signed by 35 scientists from various Chinese institutions, explains that the analysis was carried out over a period of one year and corresponds to “a first phase I clinical trial in humans that evaluates the viability of autologous transplantation of islets derived from chemically induced pluripotent stem cells (CiPSC islets) under the anterior rectum abdominal sheath for the treatment of type diabetes 1.”
What Does It Mean that Stem Cells Can Reverse Diabetes?
This stem cell transplant that has successfully reversed type 1 diabetes in a Chinese patient represents a major step forward in the treatment of this disease, which along with type 2 diabetes, is considered a chronic condition affecting more than 500 million people worldwide.
According to the World Health Organization (WHO), diabetes “is a chronic metabolic disease characterized by elevated blood glucose (or blood sugar) levels, which over time leads to serious damage to the heart, blood vessels, eyes, kidneys and nerves.”
“The most common is type 2 diabetes, which occurs when the body becomes insulin resistant or does not produce enough insulin, while type 1 diabetes −once known as juvenile diabetes or insulin− dependent diabetes is a chronic condition in which the pancreas produces little or no insulin on its own,” adds WHO.
In both cases, patients require a special diet that restricts their sugar intake and they depend on insulin treatments for survival. They also need constant medical check-ups, which entails a huge expense for both individuals and their families, as well as for public health systems. Therefore, finding a cure for diabetes can transform the lives of millions of people.
For the specific case of the Chinese patient, the paper details: “she achieved sustained insulin independence starting 75 days post-transplantation. The patient’s time-in-target glycemic range increased from a baseline value of 43.18% to 96.21% by month 4 post-transplantation, accompanied by a decrease in glycated hemoglobin, an indicator of long-term systemic glucose levels at a non-diabetic level.”
The study adds that “thereafter, the patient presented a state of stable glycemic control, with time-in-target glycemic range at >98% and glycated hemoglobin at around 5%. At 1 year, the clinical data met all study endpoints with no indication of transplant-related abnormalities.”
Although the woman has chosen to remain anonymous, it is known that she lives in Tianjin, China, is 25 years old and recently gave a telephone interview to Nature magazine in which she said: “I can eat sugar now… I enjoy eating everything, especially hotpot.”
Are There Any Other Studies to Support this Finding?
While this is the first study to reverse type 1 diabetes in a human, Nature explains that this study “follows results from a separate group in Shanghai, China, who reported in April that they had successfully transplanted insulin-producing islets into the liver of a 59-year-old man with type 2 diabetes. The islets were also derived from reprogrammed stem cells taken from the man’s own body, and he has since stopped taking insulin.”
This study was published under the title “Treating a type 2 diabetic patient with impaired pancreatic islet function by personalized endoderm stem cell-derived islet tissue” and details that the man had been diagnosed with this disease 25 years ago, but in 2017 he had a kidney transplant that worsened his health, leaving him dependent on several daily insulin injections.
According to the research, the patient received a stem cell transplant in July 2021 and 11 weeks later he no longer needed insulin injections. The study also noted that one year after the treatment, his islet cells function was restored and his kidney function was normal.
In this respect, Nature points out that there are previous investigations where “islet transplants can treat the disease, but there aren’t enough donors to meet the growing demand, and recipients must use immune-suppressing drugs to prevent the body from rejecting the donor tissue”. However, these new studies have shown that “by using tissue made from a person’s own cells, researchers also hope to avoid the need for immunosuppressants.”
Where Does the Procedure that Supports this Finding Come From?
The two investigations that have managed to reverse type 1 and type 2 diabetes in two Chinese patients, published this 2024, are based on a stem cell reprogramming technique that was developed more than 20 years ago by Japanese researcher Shinya Yamanaka at Kyoto University.
However, Nature notes that cell biologist Deng Hongkui of Beijing University, along with a group of Chinese researchers, modified this technique and “instead of introducing proteins that trigger gene expression, as Yamanaka had done, they exposed the cells to small molecules.”
By modifying this process, the Chinese scientists conducted a first test in which they “extracted cells from three people with type 1 diabetes and reverted them to a pluripotent state, from which they could be molded into any type of cell in the body.”
Initially, scientists used chemically induced pluripotent stem cells (iPS) to generate 3D islet clusters, but tested their safety in mouse and primate cells. The 59-year-old patient’s research and the 25-year-old patient’s research are therefore among the first clinical trials in humans.
About the case of the 25-year-old patient whose transplant was performed in June 2023, the operation lasted less than half an hour and “she was injected with the equivalent of approximately 1.5 million islets into her abdominal muscles.”
Previously, islets had been injected into the liver in other procedures, but the cells could not be seen there. So the researchers decided to place them in the abdomen to monitor them through magnetic resonance imaging and, if necessary, remove them.
Is this Stem Cell Treatment a Cure For Diabetes?
The authors of the research say that these are “promising results“, but warn that “more clinical studies evaluating CiPSC islet transplantation in type 1 diabetes are warranted.”
It is worth mentioning that the patient was already receiving immunosuppressants for a previous liver transplant, so scientists could not assess whether iPS cells reduced the risk of rejection of the transplant.
Jay Skyler, an endocrinologist at the University of Miami, Florida who studies type 1 diabetes, said in an interview with Nature that “it must still be verified that a woman’s cells continue to produce insulin for up to five years before she is considered cured.”
Chinese scientists have mentioned that “the results of two other participants are also very positive and will reach the mark of a year in November, after which they hope to extend the trial to another 10 or 20 individuals”, however, although hopeful, the road to a definitive cure for this disease still seems long.
Were you interested in this story? Do you want to publish it? Contact our content editor to learn more marianaleonm@tec.mx.