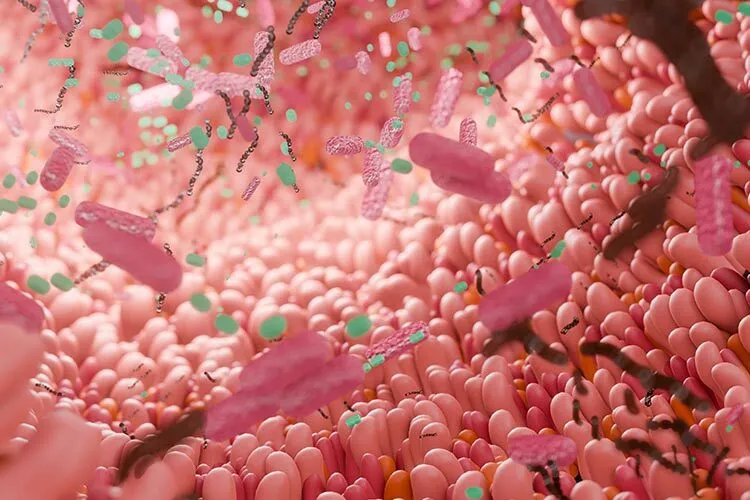
Our intestinal microbiota –the group of bacteria, fungi and viruses that inhabit our gastrointestinal tract– could explain why some people tend to have overweight or obesity.
“The combination of microorganisms that compose it carry out processes that can change from one person to another the way energy is obtained,” says Marisela González, a researcher at the Center for Research and Assistance in Technology and Design of the State of Jalisco (CIATEJ), in an interview with TecScience.
Depending on where they are located –the skin, the ears, the mouth– the organisms that conform the microbiota carry out processes that are essential for the functioning of our body. In the case of those that inhabit our intestines, they achieve metabolic activities that we cannot do on our own.
“Some examples include the synthesis of protein precursors or short-chain fatty acids and the degradation of lactose,” explains González.
In recent times, the association between the microbiota and different aspects of human health has been increasingly studied, however, most research has focused on bacteria and not so much on fungal elements such as yeasts and fungi.
Despite this, there is evidence that these elements are involved in processes such as our eating patterns, generating a need to consume foods high in sugar, for example.
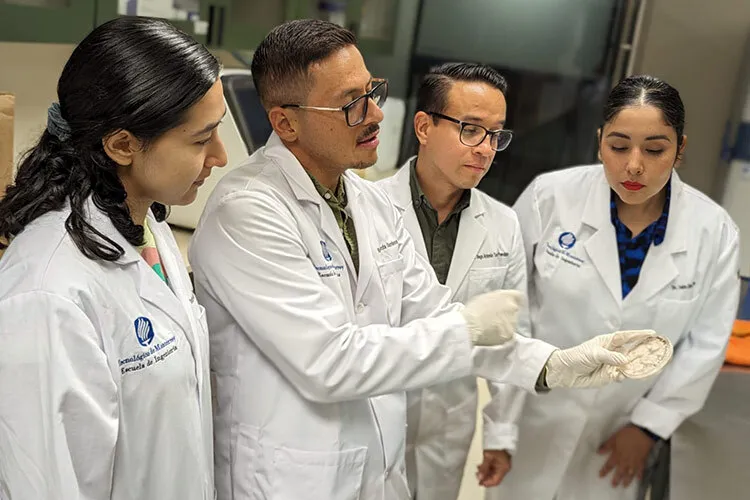
To deepen our knowledge on this subject, a group of researchers from CIATEJ, the School of Medicine and Health Sciences (EMCS) and the School of Engineering and Sciences (EIC) of Tec de Monterrey analyzed the relationship between yeasts and fungi in the intestinal microbiota and obesity.
“This could be useful for health personnel, such as nutritionists or gastroenterologists, who seek to involve the microbiota in the treatment of different conditions,” says Ricardo García, a postdoctoral researcher at the EMCS, Guadalajara Campus, who also participated in the study.
How to Study the Microbiota Fungi
Overweight and obesity are some of the biggest public health problems in Latin America and Mexico, with the latter presenting a prevalence of 75.2% in the adult population.
It is now known that obesity is complex and multifactorial, so starting to reduce its incidence will require efforts on many fronts on many fronts.
“It is not as simple as people exceeding their energy consumption, there is a direct link between the type of intestinal microbiota and weight gain,” says González.
To study this association, the researchers analyzed the microbiota of Mexican men and women, dividing them into three groups: not overweight or obese, overweight and obese.
Each one underwent an anthropometric analysis to determine their body composition, which includes the amount of fat and muscle, a biochemical blood analysis and a dietary analysis that consisted of standardized questionnaires to understand their eating patterns.
They then requested a fecal sample and sent it to the laboratory for sequencing. “There, DNA is extracted to find out which microorganisms are present in the intestine of each person,” explains García.
Using bioinformatics analysis, they put together all the data obtained and began to create microbiota profiles associated with an increase in body mass index (BMI), a parameter commonly used to detect overweight or obesity.

Distinctive Microbiota Profiles of People who are Overweight or Have Obesity
“What we found is that people with normal weight have an A pattern of microorganisms, those who are obese have a B pattern, and those who are overweight have a mix,” says González.
Some of their findings include a high prevalence of three species of fungi that can be pathogens –Candida albicans, Candida kefyr, and Rhodoturula mucilaginosa– in the intestinal microbiota of people with obesity.
For now, although their study was carried out on a small group, they can affirm that there are clear differences between the species of microorganisms that inhabit the intestine of the different body profiles.
“The fact that those who are overweight have a mix between A and B shows very clearly that weight gain is a continuous process,” says González.
This means that, with microbiota interventions, a person with obesity could lose weight. In another study they conducted with blood siblings, one of whom had obesity while the other did not, they balanced the intestinal microbiota in the individual with obesity and observed weight loss, without changing eating habits.
To perform these interventions, you first have to obtain the microbiota profile of the individual to be treated and use specific antibiotics or antifungals directed at those microorganisms that you want to eliminate or reduce, while using probiotics, prebiotics and nutraceuticals to increase the population of the positive species.
“You can also use a treatment based in probiotics and prebiotics that have antifungal or antibacterial activity,” says García. Recently, the researchers found that using probiotics that come from lactobacilli and agave inhibits the growth of Candida albicans.
The Future of Microbiota Studies
When we hear about the intestinal microbiota and its close relationship with weight gain, it is natural to wonder if these microorganisms are to blame for some people’s tendency to obesity, or if it is the other way around, where gain weight is what modifies the microbiota.
“We still don’t know which comes first, but what we do know is that these fungi, bacteria and viruses cause people to have very different digestive processes,” says González.
Although there is no normal microbiota, since “it will depend on nationality, diet and other things,” it is possible to identify species of microorganisms that could be problematic.
Interventions at the level of the microbiota of our digestive system can not only help with obesity, but also with metabolic issues, such as diabetes, or gastrointestinal diseases, such as irritable bowel syndrome.
Currently, there are some laboratories in Mexico that can sequence the DNA of the fecal sample to learn about a patient’s intestinal microbiota, however, most of the time it must be commissioned by a doctor or nutritionist who seeks to include it in a treatment.
“The intervention can be as simple as eliminating a single bacteria, or resetting the microbiota almost from scratch,” says González. “Unfortunately, in the country’s health system it is still not common.”
For the researchers, the fact that there is a trend to increasingly study the microbiota and its relationship with different diseases, ailments or conditions is something exciting, because there is still much to understand.
“Several things will be discovered about the importance of the intestinal microbiota,” says García.
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx