As we age, our movements begin to lose precision, speed, and strength. For older adults, this decline often results in reduced agility and coordination, which can lead to falls. This happens because, over time, the neurons responsible for motor skills in the brain start to deteriorate. The effects can be compounded by neurodegenerative diseases like Parkinson’s or Alzheimer’s, which further impair these abilities, even in younger individuals.
With this in mind, researchers from Tec de Monterrey and the Instituto Politécnico Nacional (IPN), working together as part of the TEC-IPN Innovation Partnerships, are collaborating on the development of a non-invasive brain rehabilitation system designed to help older adults regain mobility as they age.
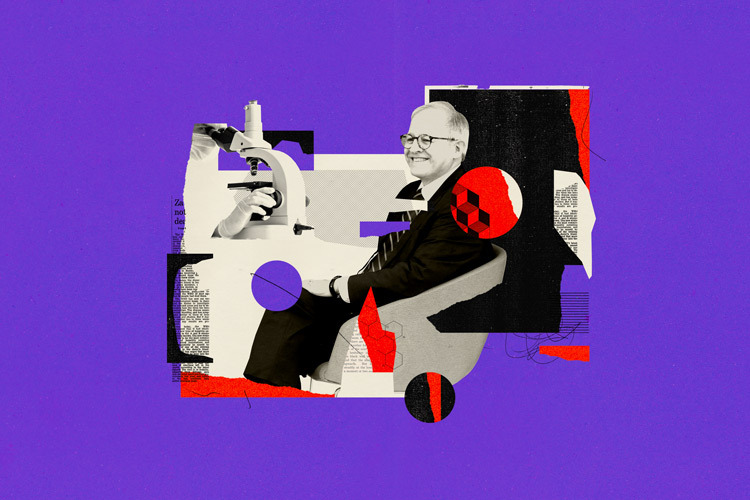
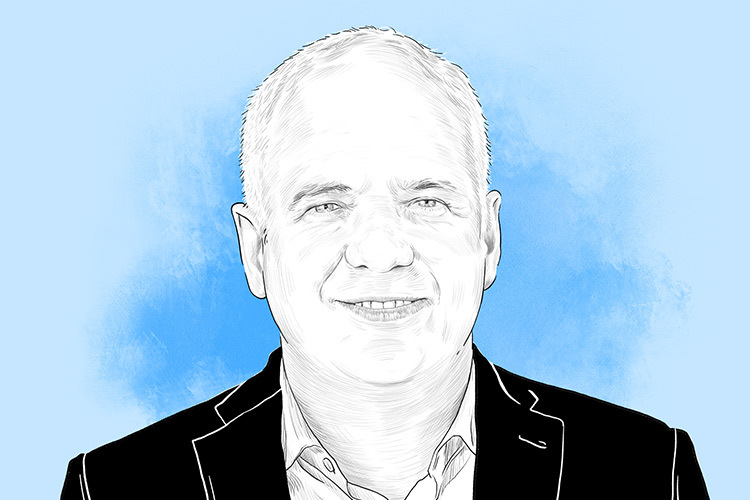
Luis Guillermo Hernández, a researcher at the School of Engineering and Sciences at Tec’s Guadalajara campus, explains that the neurorehabilitation platform combines non-invasive electrical stimulation, artificial intelligence (AI), and a robotic orthosis to simulate arm and hand movements. “We want to understand what happens to motor performance as people grow older and how we can help slow down that process,” he says.
A key element of the project is harnessing neuroplasticity—the brain’s ability to reorganize and adapt to recover lost functions. Using this technology, the researchers apply electrical stimulation to areas of the brain that have become less active over time to restore motor control.

Integrating Technologies To Identify Motor Difficulties
The system was designed by integrating three key technologies: electroencephalography (EEG), which measures brain activity; transcranial electrical stimulation (TES), which applies electrical currents to specific regions of the brain; and a robotic orthosis responsible for carrying out rehabilitation tasks. The setup also includes a computer interface with a screen that guides the patient through various exercises.
“We place a helmet on the person’s head, and through it we can both read and stimulate the brain. We also use a robotic device for the hand that allows the patient to perform exercises, like using a joystick or a mouse,” Hernández explains. The interface displays four points—up, down, left, and right—and the patient is asked to move a marker in a given direction.
This technology allows researchers to assess how fast and accurately the patient’s movements are. If tremors, slowness, or other issues are detected while performing the tasks, it becomes possible to identify signs of motor deterioration. If needed, brain stimulation can be activated as feedback.
The patient wears a cap with electrodes placed on specific points of the scalp—based on the 10-20 system—to record or stimulate activity in related brain areas. If necessary, a transcranial current—around 100 millivolts—is applied to the premotor cortex, the region directly linked to initiating movement. To determine the appropriate current level, the team follows established clinical protocols that specify the frequency, duration, and stimulation cycles to ensure the procedure remains therapeutic and non-invasive.
Hernández describes AI as the “heart” of this brain-computer interface. It interprets EEG signals to determine whether the patient is attempting to move and whether they are experiencing any difficulty. It then makes real-time decisions about how to intervene—for example, if the brain’s motor areas are not activating properly, the system sends a signal to trigger stimulation. The AI also manages interaction with the robotic device, adjusting difficulty levels or interpreting movement performance.

Validating The Technology With Older And Younger Adults
To better understand how the brain of an older adult behaves when performing basic motor tasks, the researchers conducted a series of clinical tests to measure, compare, and analyze brain activity before and after movement.
The team worked with a sample of 30 individuals over the age of 50, along with a control group of younger adults between 20 and 49 years old. During the study, they observed differences in brain activity—specifically in the beta band—between the two groups. Older adults showed latency or delayed activation in the brain region responsible for movement. The beta band refers to a range of brainwave frequencies associated with voluntary movement, focus, and motor control.
Hernández explains that the team has completed the first phase of the project, which involved characterizing the population through EEG data. The next step, phase two, is to apply and evaluate the system to determine whether the stimulation can actually improve brain performance. The goal is to identify neural biomarkers that can serve as measurable indicators in validating the platform.
“We need to give healthcare professionals a quantitative measure,” he says. “To be able to say: look, this is helping the person because this brainwave or this part of their brain is now activating 50 or 30% better.” He adds, “we’re working to identify which biomarkers in those brain signals generate meaningful feedback with this new technology.”
The project is currently at Technology Readiness Level 6 (TRL 6), meaning the prototype has been developed and is functioning at a level of technological maturity that allows for clinical testing. While the system is currently focused on upper limbs like arms and hands, it could eventually be adapted to support rehabilitation of other parts of the body.

Collaboration Between Tec and IPN Scientists
Hernández serves as the technical lead for the project at Tec de Monterrey and explains that the collaboration with researchers from IPN dates back several years, beginning with the joint development of the robotic orthosis. They secured funding for the project after winning the first TEC-IPN Innovation Partnerships grant, supported by both institutions and the Secretariat of Education, Science, Technology, and Innovation of Mexico City (SECTEI).
Throughout the development process, the teams leveraged the strengths of both institutions. “The researchers at IPN have strong expertise in prosthetics electronics and are now also collecting muscular data. On our side, we specialize in biomedical signal analysis and in creating software that integrates all these technologies—EEG, stimulation, and robotics—and delivers it to the patient,” says Hernández.
At Tec, contributors include researchers from the Neurotechnology and Brain-Computer Interface Lab, such as Javier Antelis, Joel Huegel, and Sofía Henao. From IPN, the team includes scientists from the Medical Robotics and Biosignals Lab at the Interdisciplinary Biotechnology Professional Unit (Upibi), including David Cruz and Mariana Ballesteros.
Hernández notes that for clinical validation of the platform, they also plan to involve partner institutions like TecSalud and the National Institute of Rehabilitation, with whom they’ve already collaborated on previous projects.
“We’d like to reach a point where this becomes a system people can use at home, because rehabilitation needs to be a daily, continuous process,” he says. “Another goal is to give physicians a quantitative measure to evaluate how much progress a patient has made during rehabilitation.”
Did you find this story interesting? Would you like to publish it? Contact our content editor to learn more at marianaleonm@tec.mx