Fifteen years ago, Leova Garza González, now 72, felt a tingling sensation in his left thumb. “Then I started experiencing small, uncontrollable shakes in my hand up to the wrist,” he recounts. When he went to see a doctor, they told him he might have Parkinson’s disease, starting with what they called the essential tremor, one of the early symptoms of this progressive disease. Parkinson’s gradually damages the cells of the nervous system, leading to agonizing neuronal death and its treatment remains under investigation.
In the midbrain, there is a region known as the substantia nigra. This area is critical for motor signals, learning, and body movement. The nerve cells send messages to both sides of the brain via neurotransmitters, including dopamine, which controls motor functions like moving an arm or a leg, manipulating objects precisely, or running in response to danger.

Treatment of Parkinson’s and Prevalence in Men and Women
Parkinson’s disease targets this intricate physiological mechanism. “We’re dealing with a chronic condition that has no cure, but that has treatment and can be increasingly managed and controlled,” says Héctor Ramón Martínez, a neurologist and molecular medicine expert at the TecSalud Parkinson’s and Movement Disorders Center. This institution conducts cutting-edge research and generates new knowledge to address and treat this disorder.
While Parkinson’s can occur in younger individuals, it typically appears between ages 50 and 65, affecting around 3% of the elderly population. Its incidence has doubled in the past 25 years. In Mexico, the National Institute of Neurology and Neurosurgery estimates 50 new cases per 100,000 inhabitants annually.
Age is the primary risk factor, but sex also plays a role, with men being 1.5 times more likely than women to develop Parkinson’s. The disorder has a multifactorial origin, blending environmental and hereditary causes. “In the last years of his life, my father also had it,” recalls Garza, who sought early treatment to prevent more severe symptoms.
As stated by Héctor Ramón Martínez, who has been researching this from a biological heritage perspective for two decades, “the genetic factor is present in 15% of patients with Parkinson’s, and up to 18 genes linked to its development are already known.”

Initial Symptoms
His team at the Institute of Neurology and Neurosurgery at Zambrano-Hellion Hospital is working to identify Latin American genes in patients to improve treatments to combat the disease and anticipate its most debilitating manifestations.
As he explains, “a DNA analysis is being carried out on patients with Parkinson’s to perform a genetic correlation with some clinical signs that appear and to conduct a genetic evaluation with certain markers that appear long before the disease becomes apparent.”
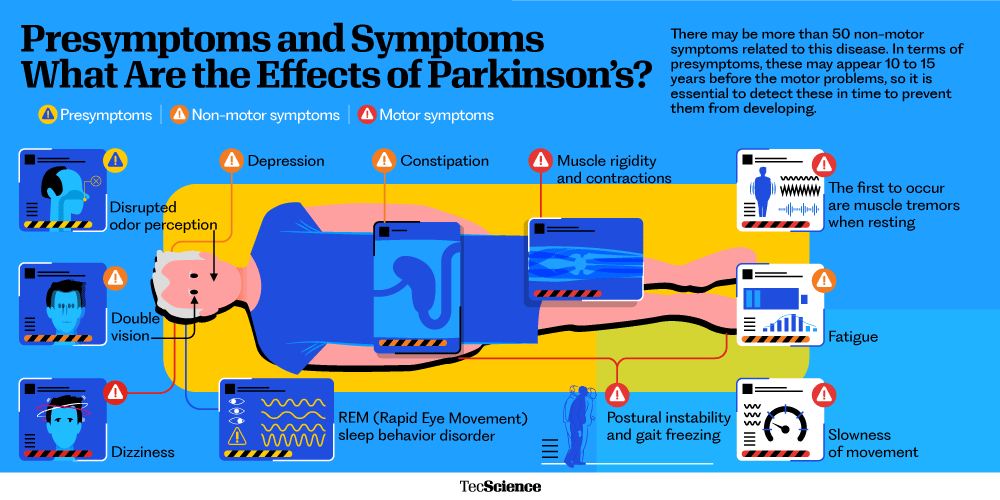
Although this neurological disorder exhibits a wide variety of data in its clinical presentation, the initial manifestation usually begins with a resting tremor, “which first occurs in one limb and then generalizes throughout the body,” the neuroscientist clarifies. Affected individuals also suffer from muscle rigidity in the limbs, slowness of movement, postural instability, and freezing.
“But there can be another 50 non-motor symptoms, such as depression and low mood, fatigue, constipation, urinary problems, and autonomic disorders,” explains Héctor Martínez. In addition to these, some signs appear up to 10 or even 15 years before motor problems, such as a loss of smell or rapid eye movement sleep behavior disorder, which causes vivid, often unpleasant dreams with a lot of action during the night, leading those affected to kick, thrash, and punch. “I wasn’t aware of it, but my wife does remember that I did it often,” confesses Leova Garza.
“With these early signs, we can predict the future development of the disease in the population and even prevent its worst effects in those we already know to have Parkinson’s,” says Martínez, one of the scientists involved in the search for biomarkers for early diagnosis. The biomarker, clinical, epidemiological, and neuropathological data analyzed in studies have shown that the pathology of this condition occurs years before the symptoms appear.
Pioneering Research
Based on this premise, TecSalud is researching microRNAs, tiny regulators of gene expression in Parkinson’s patients. “The levels and content of these microRNAs in patients’ blood can track the disease’s progression,” Martínez says. These molecules, secreted as messengers in bodily fluids, are promising biological indicators.
MicroRNAs have become an attractive non-invasive tool for diagnosing early and monitoring the progression of neurodegenerative diseases. “If we find recurring microRNAs in Parkinson’s patients associated with pre-symptoms, we can intervene before motor symptoms start,” Martínez details.
As Héctor Ramón Martínez explains, the levels in a patient’s blood and the content of their information can be used to track the course of the disease. “These micro-regulators found in bodily fluids and other extracellular environments, such as plasma, serum, urine, cerebrospinal fluid, and saliva, are actively secreted as messengers, exhibiting a complex cell-to-cell communication mechanism.” This property has positioned them as potential biological indicators.
In recent years, microRNAs have become an attractive non-invasive tool for early diagnosis of neurodegenerative diseases, both for monitoring and progression. “If we find forms of microRNA that are repeated in Parkinson’s patients and are related to some of the early signs before the initial presentation of the disease is detected, we can intervene before motor symptoms begin. That is, before more than 50% of the dopaminergic neurons are lost,” Martínez explains.
“Thanks to starting treatment early, my symptoms are minor. My hands still tremble if I get nervous or angry. However, I can still drive and draw,” says patient Leova Garza, who did not give up his profession as an architect despite the stark diagnosis he received over a decade ago. “When the death of nerve cells progresses, the chances of helping the patient and treating them as soon as possible with the available therapies diminish,” notes Martínez, one of the doctors who has been treating him since then.
The Era of Stimulation Treatments
Current medications for Parkinson’s, like levodopa, have been in use since the 1960s. This dopamine precursor helps with movement and coordination. “These drugs work well when combined with physical activity and rehabilitation,” says Martínez.
When medications and motor rehabilitation therapies are no longer effective, it’s time to turn to stimulation techniques, explains Fortino Salazar, a neurosurgeon and co-founder of the TecSalud Parkinson’s Center.
Since 2000, Salazar’s team has operated on patients with severe, medication-resistant tremors. Annually, about 20 individuals undergo DBS at the center.
This technique uses electrical current to regulate brain activity by placing electrodes in the brain and a battery under the chest, functioning like a pacemaker. “This allows for significant control of rigidity, tremor, or slowness, among other symptoms,” explains Fortino Salazar. Leova Garza, who underwent the surgery more than a year ago, says it changed his daily life, “I noticed a 100% difference,” the patient asserts.
The neurosurgeon who treated him explains, “With this intervention, a significant improvement in the patient’s quality of life is anticipated, and a 50% average reduction in the required medications is expected, which also reduces side effects.”
“Over time, the amount of levodopa I was taking increased for it to be effective. But I didn’t want to take so many pills. I reduced them by up to 90% thanks to the surgery!” Garza is grateful for the significant changes he noticed after undergoing Deep Brain Stimulation.

Spinal Stimulation Technologies
“This is a safe therapy that works very well. However, it does not improve all issues, such as walking,” clarifies Eduardo Moraud, referring to Deep Brain Stimulation. This Spanish scientist works at the Swiss Federal Institute of Technology in Lausanne and is one of the world’s leading experts in neuromodulation techniques.
For over a decade, Moraud has applied his engineering and robotics expertise to studying the human nervous system, becoming a pioneer in spinal stimulation technologies. “Instead of sending activation to the brain area affected by Parkinson’s, we stimulate the spinal cord. In other words, we do not attack the origin of the problem. Still, the output that sends signals to the legs,” explains the research group leader responsible for a historic milestone: enabling a patient with advanced Parkinson’s disease to walk again.
This revolutionary technique had already been tested on paraplegic individuals who were unable to take a single step and, after the intervention, regained their ability to walk the day after the operation.
In 2021, the interdisciplinary team led by the Spaniard succeeded in implementing the same type of neuroprosthesis in a Swiss patient who had been living with the disorder for more than 20 years. “He had already undergone deep brain stimulation and other available techniques that improved his symptoms. But there came a point when he no longer responded to therapies and could no longer walk,” explains the scientist, who then came up with the idea of installing two implants in his brain to read thoughts and send them to a third implant to electrically stimulate the spinal cord.
After the implementation of his development, “our patient went from falling up to six times a day to at most once a week. In addition to improving his physical condition, he began to feel much more confident,” Moraud details.
The revolutionary technology can measure the electrical activity generated by the brain to control spinal stimulation, acting as a digital bridge between the brain and the spine, the key elements for any motor activity.
“In a healthy person, the brain sends signals to the spinal cord to restore voluntary control. When there is some problem in the brain, the implant helps us trick the faulty nervous system, manipulating these connections to appropriately stimulate the spinal cord and enable the patient to walk,” explains the engineer, proud of the impact of this historic development.
Incorporating innovative techniques
Recently, TecSalud successfully incorporated a new technology into DBS in a 65-year-old patient with advanced Parkinson’s. This device sends electrical impulses and detects and corrects altered brain activity, improving the patient’s clinical state.

“With this device, in addition to sending the electrical impulses to the brain, we can detect altered brain activity in patients and correct it in real time. This allows for more precise stimulation and improves the patient’s clinical condition,” explains the neurosurgeon at TecSalud, the only private center in the country that offers the most effective and innovative methods for managing Parkinson’s, positioning itself among the best care centers in the world.
“We already have a protocol that we will apply to use Spinal Stimulation in these patients with walking difficulties, which we use for other conditions, such as chronic pain,” explains Fortino Salazar. His team also plans to incorporate another revolutionary development into their services. “This involves high-intensity focused ultrasound, the well-known HIFU technique, which does not require surgery and is only available in very few places worldwide,” he notes.

This innovative treatment uses ultrasound waves to treat debilitating tremors with a non-invasive procedure. “It produces the same effects as deep brain stimulation to improve slowness, rigidity, or tremors,” says Martínez.
Social Implications of Parkinson’s
Remember that this disorder completely disables daily activities, from dressing to eating. Everyday tasks that take increasingly longer for those who suffer from it, and that, as the disease progresses, end up becoming an impossible mission,” says the neurologist, who explains that the course of Parkinson’s on many occasions causes the person to isolate themselves and enter a depression.
Leova Garza has worked to alleviate the social effects of the disease he has suffered from for 15 years. “Before, when I got the shakes, I would hide the hand I couldn’t control. I wanted to avoid giving explanations and feeling sorry for myself. I don’t do that anymore,” he reveals.
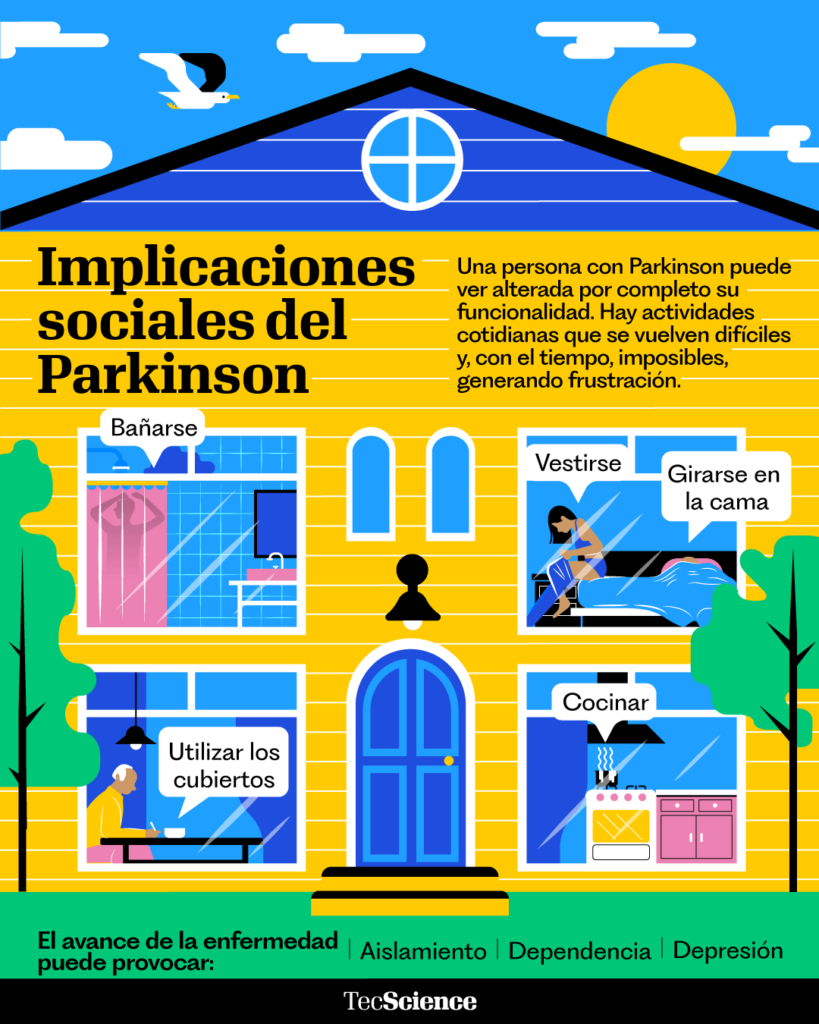
“The social implications of Parkinson’s are immense. Therefore, the importance of patient care must be under the coordination and experience of a multidisciplinary team, which integrates from neurosurgery specialists to psychologists,” says Martínez. In his opinion, this positions TecSalud as one of the best centers for treating the disease: “The close accompaniment of patients and their families together with the implementation of the most effective and pioneering therapies based on frontier science.”
Although the mechanisms of Parkinson’s still hold many unknowns for medicine, “and there is a long way to go to stop it completely, I do not doubt that we will achieve it soon,” Salazar enthusiastically assures. At the moment, his team has already achieved that patients like Garza, with more than a decade living with the disorder, can control almost all of its sequelae and, as the architect himself confesses, “recover the quality of life thanks to the wonderful care that the entire medical team provided me.”
Interested in this story? Want to publish it? Contact our content editor to learn more: marianaleonm@tec.mx.








