By Ana Sofía González Quintanilla / Amateur Science
Reviewed by Jorge Eugenio Valdez García
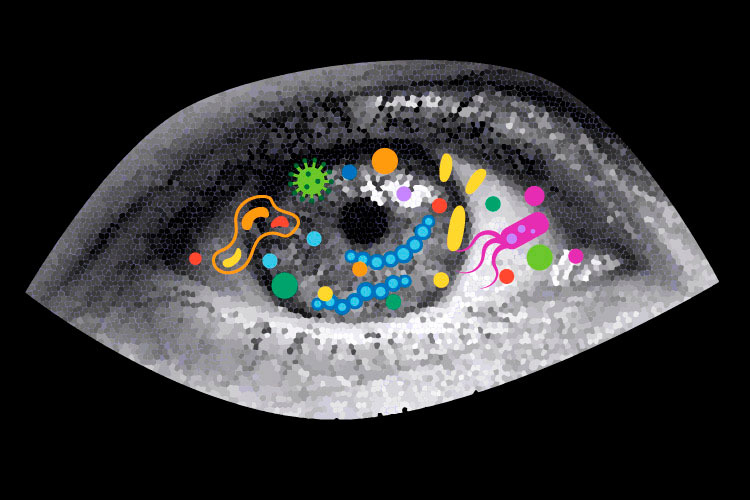
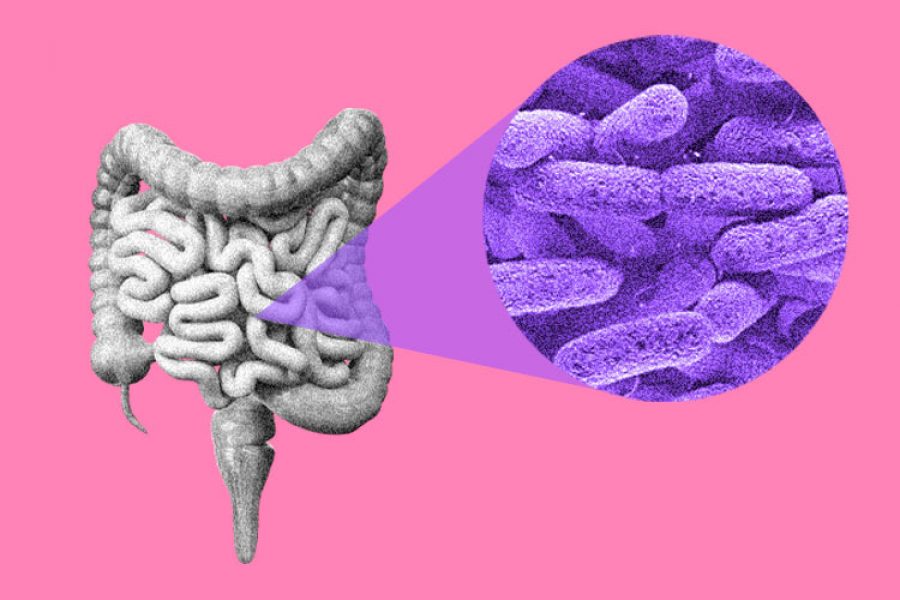
You may not notice it, but a community of microbes lives in your eyes, working quietly to keep them healthy. This is the ocular microbiota—a group of bacteria, fungi, and viruses that play a crucial role in protecting and maintaining the proper function of your eyes.
While less well-known than the gut or skin microbiota, the ocular microbiota is essential for eye health. It acts as the first line of defense against infections and helps to maintain stability.
What is the Ocular Microbiota?
The ocular microbiota refers to the microorganisms that inhabit the eye’s surface, specifically the conjunctiva (the membrane surrounding the eye) and the cornea, the transparent layer covering the eye in front of the iris and pupil.
These microorganisms do not cause eye diseases in healthy individuals.
The human eye is constantly exposed to the external environment, so it might seem more susceptible to infections than other organs. However, thanks to tears and our immune system, we are protected.
Only a specific group of microorganisms survive on the eye’s surface. They coexist in balance with the body and usually do not cause harm. However, when the ocular microbiota becomes imbalanced—due to factors like surgeries, certain medications, or dry eye syndrome—it can lead to infections. Understanding this delicate balance is key to preserving eye health.
Bacteria, Fungi, and Viruses in the Eye
The ocular microbiota primarily consists of bacteria, but fungi and viruses can also be present. Common bacteria include Staphylococcus epidermidis, which protects against harmful microbes; Propionibacterium acnes, which may cause skin conditions but does not harm the eye; Corynebacterium spp., which supports the immune system; and Staphylococcus aureus, which, when overabundant, can lead to infections.
Fungi like Candida spp. and viruses, such as certain herpes viruses, can also be present, typically remaining dormant without causing issues. The role of these microorganisms largely depends on the balance in the eye.
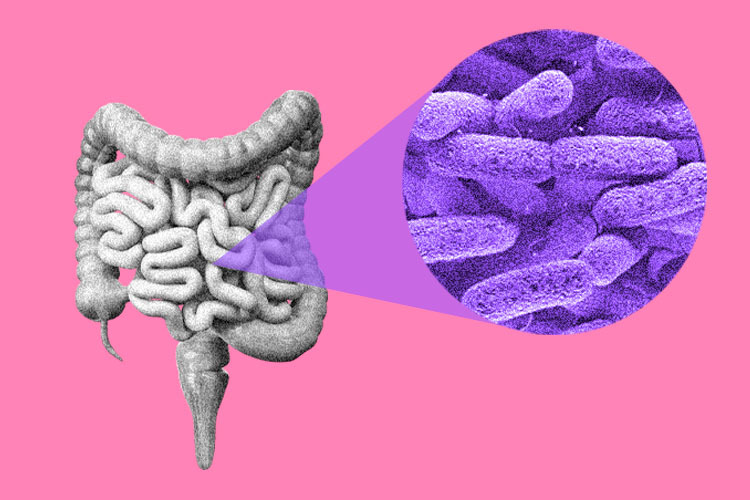
The ocular microbiota is not passive; it plays a vital role in maintaining eye health. These bacteria help protect against infections by competing with harmful microbes and producing substances that block dangerous bacteria, such as Pseudomonas aeruginosa.
They also work with the body’s immune system by signaling and teaching it to distinguish between good and bad microorganisms, preventing unnecessary inflammation. Additionally, they help keep the eyes moist and clean by stabilizing the tear film and promoting cell regeneration in the cornea and conjunctiva.
This natural balance is a great example of how our body and microorganisms collaborate to protect our health.
When the Balance is Disrupted
Contact lens use, overuse of antibiotics, diabetes, hormonal changes, and exposure to pollutants like dust and smoke can disrupt the ocular microbiota.
These disruptions can increase the risk of issues such as blepharitis (inflammation of the eyelids), keratitis (corneal infection), and bacterial conjunctivitis. In dry eye syndrome, changes in the microbiota are often linked to chronic inflammation, which can exacerbate the condition.
This “natural shield” can also be compromised by poor hygiene or excessive use of certain eye drops, leaving the eye more vulnerable to infections.
Research is advancing in the study of the ocular microbiota, paving the way for new treatments for various eye diseases. For example, probiotics in eye drops—similar to those used for gut health—are being explored to help restore the balance of microorganisms when imbalances affect eye health.
Researchers are also focusing on personalized therapies, analyzing the specific composition of each person’s ocular microbiota to create more targeted and effective treatments.
Genomics is being employed to study the genes of microorganisms in the eye, helping to identify new ways to diagnose and treat diseases earlier and more efficiently.
These advances in ophthalmic research could improve eye health and revolutionize eye care, making treatments more personalized and effective.
References
- Graue-Wiechers, E., Valdez-García, J., Muñoz-Salas, S., Islas-de la Vega, G., & Curiel, J. de J. (1990). Evaluación de la flora bacteriana en ojos de cadáver: Sus variables y métodos de asepsia. Revista Mexicana de Oftalmología, 64(6), 209–213.
- Gomez-Elizondo, D. E., Lopez-Martinez, M., Ruiz-Lozano, R. E., Valdez-Garcia, J. E., & Hernandez-Camarena, J. C. (2021). Corneal perforation associated with isolated ocular lichen planus: A case report. European Journal of Ophthalmology, 31(6), NP9–NP12.
- Domene-Hickman, J. L., Torres-Gómez, J., Valdez-García, J. E., Hernández-Camarena, J. C., Ortiz-Morales, G., & Domene Hinojosa, J. L. (2020). Queratitis fúngica de inicio tardío por Candida glabrata posterior a queratoplastia penetrante. Revista Mexicana de Oftalmología, 94(6), 284–288.
- Valdez-García, J. E., Climent, A., Chávez-Mondragón, E., & Lozano-Ramírez, J. F. (2014). Anterior chamber bacterial contamination in cataract surgery. BMC Ophthalmology, 14, 1–4.
- Grzybowski, A., Schwartz, S. G., Matsuura, K., Tone, S. O., Arshinoff, S., Ng, J. Q., Meyer, J. J., Liu, W., Jacob, S., Packer, M., Lutfiamida, R., Tahija, S., Roux, P., Malyugin, B., Urrets-Zavalia, J. A., Crim, N., Esposito, E., Daponte, P., Pellegrino, F., … Behnding, A. (2017). Endophthalmitis prophylaxis in cataract surgery: Overview of current practice patterns around the world. Current Pharmaceutical Design, 23(4), 565–573.
- Torres, J., Ibarra-Lozano, A. F., Gonzalez, P. M., & Valdez, J. E. (2015). Susceptibility and resistance of Staphylococcus epidermidis ocular strains in a Hispanic population. Investigative Ophthalmology & Visual Science, 56(7), 267–267.
- González, P. M., Ibarra-Lozano, A. F., Valdez, J. E., & Torres, J. (2015). Pseudomonas aeruginosa ocular strains resistant to ceftazidime in Northeast of Mexico. Investigative Ophthalmology & Visual Science, 56(7), 4049–4049.
- Willcox, M. D. P. (2013). Characterization of the normal microbiota of the ocular surface. Experimental Eye Research, 117, 99–105.
- El Hajjioui El Ouassaidi, S. (2024). Microbioma ocular y salud visual (Master’s thesis, Universitat Politècnica de Catalunya).
Author
Ana Sofia Gonzalez Quintanilla. Medical student at Tecnológico de Monterrey.
Reviewer
This article was reviewed by Jorge Eugenio Valdez García, an ophthalmologist and subspecialist with a Master’s degree in Medical Sciences and a Ph.D. in Surgical Research. He is a professor and head of the Cornea and Refractive Surgery Service at the Institute of Ophthalmology and Visual Sciences at the Zambrano Hellion Medical Center of TecSalud. He is the leader of the Innovative Ophthalmology and Visual Sciences Research Group (GIEE) at the School of Medicine and Health Sciences at Tecnológico de Monterrey. He is a member of the National System of Researchers, Level 2, and a Mexican Academy of Surgery member.