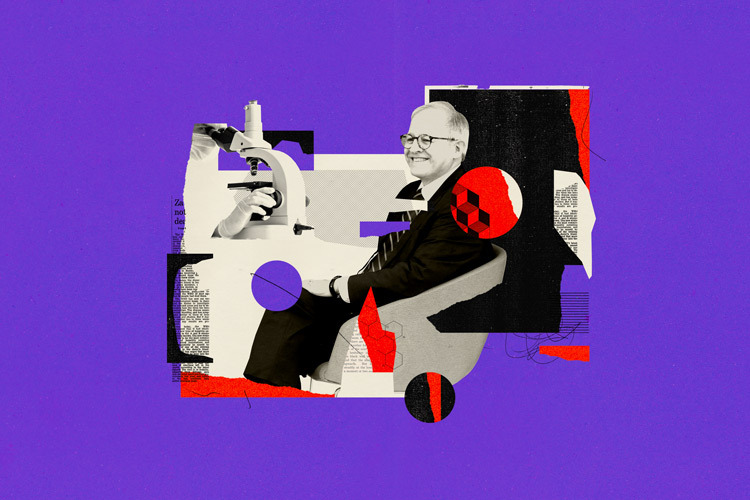
Do early adverse childhood experiences (ACEs) have a lasting effect on physical health later in life? A team of researchers at Tecnológico de Monterrey is working on a project that seeks to draw connections between the psychological toll of these stressful events and a heightened risk of developing conditions like obesity, diabetes, or hypertension—by analyzing biological samples such as hair, saliva, stool, urine, and blood.
ACEs are traumatic events that—without proper support—can disrupt the healthy development of children. These include physical, sexual, or emotional abuse; physical and emotional neglect; witnessing domestic violence; or having family members with addictions, mental illness, or who are incarcerated.
Alejandra Chávez Santoscoy, a research professor at the School of Engineering and Sciences (EIC) and head of the Core Lab: Genomics, explains that the project titled Search for microbiome biomarkers associated with adverse events in children’s mental health for early prevention and diagnosis takes both a sociodemographic and biological approach to understand how ACEs can leave a physical imprint on children.
“Maybe we can’t prevent a child from going through an adverse experience,” Chávez says, “but we can try to reduce the impact it has on their health.” The project brings together researchers from EIC and the School of Medicine and Health Sciences (EMCS), in collaboration with the Tec’s Center for Early Childhood and Fundación FEMSA.
Preliminary results show that children who experienced more adversity tend to have higher levels of pathogenic microorganisms in their microbiome—some linked to cavities, periodontitis, and inflammation. Meanwhile, those with a significant number of positive, nurturing experiences showed a stronger presence of beneficial microorganisms that support immune and gut health, such as lactobacilli.
The physiological impact of ACEs
According to the First National Survey on Adverse Childhood Experiences conducted by the Early Childhood Center, nine out of ten Mexican adults experienced at least one ACE during their childhood, and 22.6% went through more than four. “Having more than four adverse experiences is linked, for instance, to a higher risk of obesity, diabetes, and hypertension—and the odds are even greater: eight times higher for suicide and six times higher for major depression.”
Chávez points out that, until now, Mexico lacked enough data to clearly determine whether childhood experiences had a measurable impact on physical health. What’s more, most current prevention strategies focus on health issues once people have already reached adulthood. By incorporating biological analysis into the findings of the national survey, this study will offer a clearer picture of how ACEs affect children’s health—and pave the way for solutions, early diagnoses, and timely interventions starting in childhood.
The study involves the collection of non-invasive biological samples to identify biomarkers linked to health problems. For example, hair samples are used to measure cortisol levels—the so-called stress hormone—which is also present in children but can have a stronger impact due to their limited ability to regulate emotions at a young age. The exact amount of cortisol accumulated over time is determined using spectrophotometric analysis to assess chronic stress levels.
As part of the collection process, the team is also studying two types of microbiota. Oral microbiota is gathered through saliva samples or buccal swabs, and gut microbiota is analyzed using stool samples. Genetic sequencing helps determine the bacterial composition in the gut and detect the presence of harmful microorganisms, deficiencies in beneficial bacteria, or imbalances associated with issues like chronic inflammation, colitis, or a predisposition to obesity. “The microbiota acts like a mirror of the child’s condition—even when parents might not notice anything is wrong,” Chávez explains.
The research team also analyzes blood samples using techniques such as ELISA (Enzyme-Linked ImmunoSorbent Assay) to detect proteins and molecules of the immune system, as well as markers of chronic inflammation—like interleukins and TNF-α. These markers are associated with metabolic diseases such as obesity and diabetes, and with psychological conditions including depression and long-term chronic stress.
Cross-referencing biological samples with sociodemographic data
The project’s methodology also includes gathering information about the child’s family, social, and environmental context. This data is then cross-referenced with the biological samples and other anthropometric measurements, such as weight, height, and body mass index, that help assess the child’s overall health.
This information is collected through surveys completed by parents or guardians, in which they report their own adverse experiences as well as those they’ve observed in their children. The surveys also ask about household characteristics, dietary habits, medication or antibiotic use, and other relevant factors. “Once we have all the data, we try to correlate what the parent reported with what we’re seeing biologically in each of the markers,” Chávez explains.
One of the biggest challenges the project has faced is the cost—each full analysis is estimated at around 15,000 pesos, at minimum. Because of this, the study initially focuses on a regional level, within the Monterrey metropolitan area, through a partnership with the Centros de Desarrollo Infantil (CENDI)—early childhood care and education centers. There, 100 parent-child pairs participated, meaning 200 samples were collected in total. The children were between 3 and 5 years old.
Early childhood as a “window for early intervention”
Chávez emphasizes that the goal is to intervene early. While it’s still unclear exactly when adversity begins to cause harm to a child’s health, this particular stage of development was chosen because it represents a window for early intervention—when the effects of chronic stress can still be reversed. In other words, if we can identify which children are beginning to show signs of health issues due to adverse experiences, we could potentially prevent many of the diseases that currently overwhelm public health systems.
The outcomes of this project could have clinical, nutritional, and public health implications. These might include incorporating emotional and social dimensions into medical guidelines; developing functional diets, probiotics, and personalized foods for children in vulnerable environments; and investing in the prevention of conditions like diabetes, obesity, hypertension, and depression.
However, even though all the biological samples have already been collected for the study, additional resources are still needed to complete the analysis—which is currently about halfway through. “We would love to see this project carried out at a national level,” says Chávez, “but at the end of the day, these biological samples come with a cost that makes scaling up a real challenge. If we invest in early childhood, we can ease the burden of health problems we see later in the adult population.”
Were you interested in this story? Do you want to publish it? Contact our content editor to learn more marianaleonm@tec.mx.